Peptic ulcer disease isn’t just a bad stomach ache. It’s a real break in the lining of your stomach or upper intestine - deep enough to expose sensitive tissue to stomach acid. About 8 million people worldwide deal with it every year. For decades, people blamed stress, spicy food, or too much coffee. But since 1982, we’ve known the real culprits: H. pylori bacteria and common painkillers like ibuprofen and aspirin.
What’s Really Causing Your Ulcer?
Most peptic ulcers come from one of two places: infection or medication. H. pylori is a spiral-shaped bacterium that lives in the stomach lining. It doesn’t just survive in acid - it digs in, weakens the protective mucus layer, and triggers inflammation. About 50% of people with duodenal ulcers and 30-50% with gastric ulcers have this infection, according to Merck Manuals.
The other big cause? NSAIDs - nonsteroidal anti-inflammatory drugs. That includes ibuprofen (Advil, Motrin), naproxen (Aleve), and even low-dose aspirin taken daily for heart health. These drugs block enzymes that help protect the stomach lining. In fact, NSAIDs now cause more than half of all peptic ulcers, especially in older adults who rely on them for arthritis or chronic pain.
Smoking and heavy drinking make things worse. Smokers are 2 to 3 times more likely to develop ulcers. People who drink more than three alcoholic drinks a day raise their risk by 300%. Stress doesn’t cause ulcers directly, but it can slow healing and make symptoms feel worse.
How Do You Know You Have One?
The classic sign is a burning or gnawing pain in the upper abdomen - right below the breastbone. It often comes on when your stomach is empty, like between meals or at night. Some people say eating or taking antacids makes it better. Others feel full fast, get nauseous, or can’t tolerate greasy foods.
But red flags mean you need help right away: vomiting blood (looks like coffee grounds), black or tarry stools, sudden sharp stomach pain, or unexplained weight loss. These could mean bleeding, a hole in the intestine, or a blockage. Don’t wait. Go to a doctor.
Diagnosis isn’t guesswork. You’ll need an endoscopy - a thin camera passed down your throat to see the ulcer. Doctors will also test for H. pylori using a breath test, stool sample, or biopsy during the endoscopy. Blood tests aren’t reliable for current infections because they show past exposure, not active bugs.
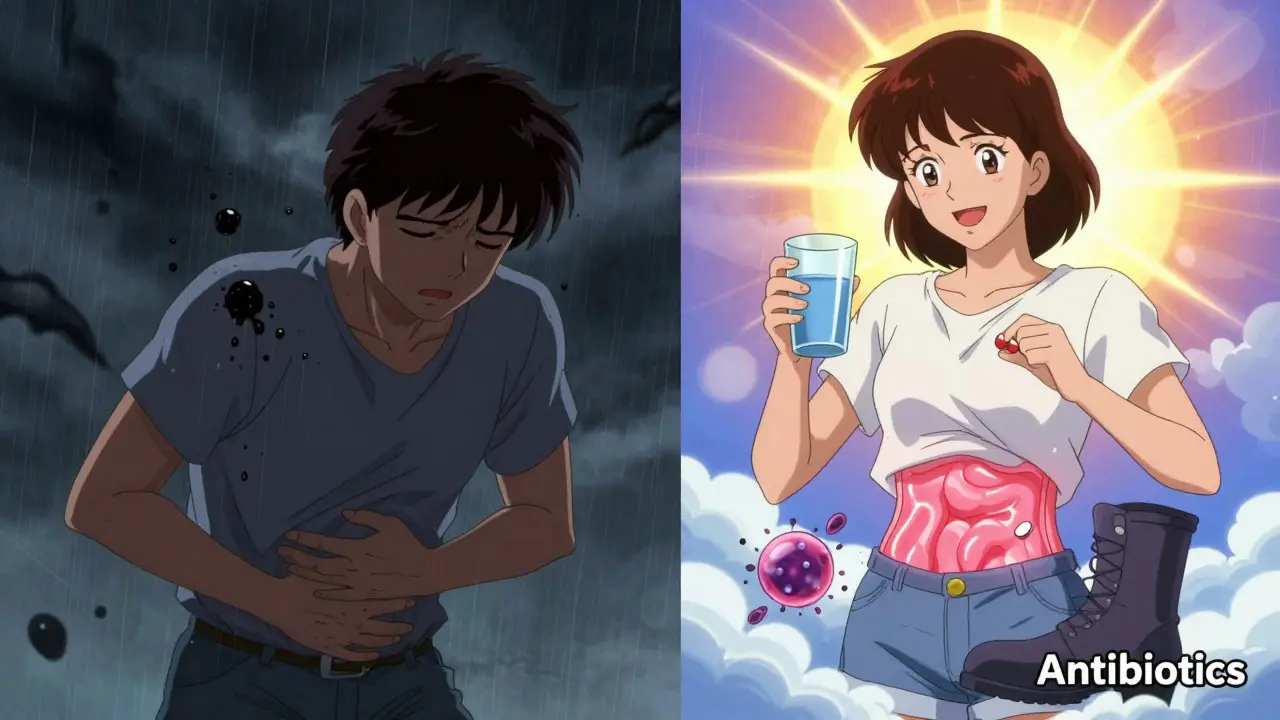
Antibiotics: The Real Cure for H. pylori
If you have an H. pylori infection, antibiotics are your best shot at a permanent fix. Without them, ulcers come back in 70% of cases. With them? Down to 10%.
The standard treatment is called triple therapy: two antibiotics plus a proton pump inhibitor (PPI), taken for 7 to 14 days. Common combos include:
- Pantoprazole + clarithromycin + amoxicillin
- Pantoprazole + clarithromycin + metronidazole
- Lansoprazole + amoxicillin + metronidazole
Some places now use quadruple therapy - adding bismuth (like Pepto-Bismol) - especially where clarithromycin resistance is high. In the U.S., resistance is now over 35%, so this is becoming first-line in many clinics.
Side effects are common. Many people get diarrhea, nausea, or a strange metallic taste - especially with metronidazole. Some feel dizzy or lose their appetite. But here’s the catch: skipping doses or stopping early is the #1 reason treatment fails. You have to finish the full course, even if you feel better after day three.
After treatment, your doctor will retest you - usually with a stool test - to make sure the bacteria are gone. If it’s still there, they’ll try a different antibiotic combo.

Acid-Reducing Medications: Letting the Ulcer Heal
Antibiotics kill the bug, but acid-reducing drugs give your lining time to heal. Two types are used: proton pump inhibitors (PPIs) and H2 blockers.
PPIs are the gold standard. They shut down acid production almost completely for 24 to 72 hours. Common ones include:
- Omeprazole (Prilosec)
- Esomeprazole (Nexium)
- Lansoprazole (Prevacid)
- Pantoprazole (Protonix)
- Rabeprazole (AcipHex)
They work best when taken 30 to 60 minutes before breakfast - sometimes before dinner too. Taking them with food reduces their effect.
H2 blockers like famotidine (Pepcid) and cimetidine (Tagamet) help too, but they’re weaker. They only block acid for 10 to 12 hours. Most doctors now use them only if PPIs aren’t tolerated.
Patients on Drugs.com rate omeprazole at 6.2/10, esomeprazole at 6.8/10. About half say they work well. But long-term use? That’s where concerns pop up. The FDA warns about possible risks: lower vitamin B12 levels, higher fracture risk in older adults, and rare kidney issues. That’s why doctors don’t recommend PPIs longer than needed.
What If You Can’t Stop Taking NSAIDs?
If you’re on daily aspirin for your heart or ibuprofen for arthritis, stopping isn’t always an option. In that case, your doctor might:
- Switch you to a COX-2 inhibitor like celecoxib (Celebrex) - easier on the stomach
- Prescribe a PPI long-term to protect your lining
- Recommend misoprostol (Cytotec), a drug that replaces protective prostaglandins
Some people switch to acetaminophen (Tylenol) for pain. It doesn’t harm the stomach lining like NSAIDs do. But don’t take more than 3,000 mg a day - too much can damage your liver.
What About Rebound Acid?
Many people who stop PPIs suddenly notice their heartburn comes back - worse than before. That’s called rebound acid hypersecretion. Your stomach overcompensates after being quiet for weeks. It’s not dangerous, but it’s uncomfortable.
The fix? Don’t quit cold turkey. Work with your doctor to slowly lower the dose over a few weeks. Sometimes switching to an H2 blocker for a bit helps ease the transition.
The Future: Faster, Smarter Treatment
There’s new hope on the horizon. In January 2023, the FDA approved vonoprazan - a new type of acid blocker called a potassium-competitive acid blocker. It works faster and stronger than PPIs, with eradication rates hitting 90% in trials. It’s already used in Japan and is starting to show up in U.S. clinics.
Doctors are also moving toward personalized treatment. Instead of guessing which antibiotics will work, they’re testing for bacterial resistance before prescribing. By 2025, 60% of H. pylori treatments are expected to be guided by these tests - up from just 15% in 2022.
Even with better drugs, lifestyle matters. Quit smoking. Cut back on alcohol. Avoid NSAIDs unless necessary. Eat regular meals. Stress won’t cause ulcers, but it can delay healing.
Final Takeaway
Peptic ulcer disease is no longer a life sentence. It’s one of the most treatable conditions in gastroenterology. If you have symptoms, get tested for H. pylori and review your meds. Antibiotics can cure the root cause. PPIs let your body heal. And if you’re on NSAIDs long-term, there are safer ways to manage it.
The key? Don’t ignore the pain. Don’t stop meds early. And don’t assume it’s just ‘indigestion.’ With the right approach, most people are symptom-free in weeks - and ulcer-free for good.
Can stress cause peptic ulcers?
No, stress doesn’t directly cause peptic ulcers. The main causes are H. pylori infection and NSAID use. But stress can slow healing and make symptoms feel worse, so managing it helps.
Do I need to take antibiotics if I have an ulcer?
Only if you have an H. pylori infection. Your doctor will test for it. If it’s positive, antibiotics are essential to prevent recurrence. If your ulcer is from NSAIDs, antibiotics won’t help - you’ll need to stop the meds and use acid reducers instead.
How long do I need to take PPIs for an ulcer?
Typically 4 to 8 weeks for healing. If you have H. pylori, you’ll take PPIs during and after the 7-14 day antibiotic course. Long-term use (more than 8 weeks) should be reviewed by your doctor due to potential side effects.
Can I drink alcohol with a peptic ulcer?
No. Drinking more than three alcoholic drinks a day increases your ulcer risk by 300% and slows healing. Even moderate alcohol can irritate the stomach lining. Avoid it until your ulcer is fully healed and your doctor says it’s safe.
Is it safe to take omeprazole long-term?
For most people, short-term use (4-8 weeks) is very safe. Long-term use (over a year) may increase the risk of vitamin B12 deficiency, bone fractures, or rare kidney issues. If you need ongoing acid control, your doctor may switch you to the lowest effective dose or try H2 blockers.
What’s the best painkiller if I have a history of ulcers?
Acetaminophen (Tylenol) is the safest choice. It doesn’t damage the stomach lining like NSAIDs do. Avoid ibuprofen, naproxen, and aspirin unless your doctor says it’s okay - and even then, you’ll likely need a PPI on the side.
Can peptic ulcers turn into cancer?
Rarely. Long-standing H. pylori infection increases the risk of stomach cancer, but the chance is still low - less than 1% over a lifetime. Treating the infection early removes most of that risk. Regular follow-up with your doctor is key if you’ve had a gastric ulcer.


Comments (15)
Martin Spedding December 16 2025
h. pylori? more like h. bullsh*t. my uncle had ulcers for 10 yrs, doctors said stress, then one day some guy in a lab said "oh btw its bacteria". now he's fine. why did it take so long??amanda s December 17 2025
AMERICA STILL USING CLARITHROMYCIN? WE'VE BEEN ON QUADRUPLE THERAPY SINCE 2019. YOU GUYS ARE STILL LAGGING BEHIND. THIS IS WHY OUR HEALTHCARE IS A JOKE.Anu radha December 19 2025
i had ulcer last year. pain like fire. doctor gave me antibiotics. i felt better after 3 days. but i took all pills. now no pain. thank you medicine.Salome Perez December 20 2025
It's truly remarkable how far we've come-from blaming spicy tacos and midnight stress-eating to pinpointing a tiny spiral-shaped bacterium as the root cause. The science here is elegant, and the treatment protocols? Almost poetic in their precision. Kudos to the researchers who refused to accept the old myths.Pawan Chaudhary December 21 2025
you got this! i know it feels overwhelming but antibiotics + ppi is your new best friend. stick with it. your stomach will thank you later 😊BETH VON KAUFFMANN December 21 2025
The FDA warning on PPIs is underplayed. Long-term use correlates with hypomagnesemia, C. diff, and increased all-cause mortality in observational cohorts. The risk-benefit calculus needs recalibration, especially in asymptomatic GERD patients on indefinite therapy.Donna Packard December 22 2025
i never knew stress didn't cause it. i thought i was just too anxious. learning this changed everything for me.Patrick A. Ck. Trip December 22 2025
i think the real issue is how long we let misinformation persist. h. pylori was discovered in '82. why did it take 20 years for most docs to test for it? i'm not blaming anyone, but... it's frustrating.Sam Clark December 23 2025
The integration of resistance-guided therapy represents a paradigm shift in antimicrobial stewardship. By aligning treatment regimens with local resistance epidemiology, we reduce unnecessary antibiotic exposure and improve eradication efficacy. This is precision medicine in action.Jessica Salgado December 25 2025
i just got diagnosed. i cried. not because of the ulcer... but because i finally understood why my stomach has been screaming for years. thank you for writing this. i feel less alone.Kaylee Esdale December 25 2025
antibiotics are hard but worth it. i took mine with peanut butter to hide the taste. also drink water. lots of water. your gut will thank youJody Patrick December 25 2025
in india, many people still think chili causes ulcers. we need more education. this post is very helpful.Erik J December 26 2025
I read this whole thing and still don't know if my daily aspirin is the problem. I take 81mg for heart. Should I stop? Or just take omeprazole forever? No one ever told me the trade-offs.Brooks Beveridge December 26 2025
Hey, you're not alone. I was in the same boat. Took the full 14-day triple therapy, hated the metallic taste, almost quit on day 5. But I stuck with it. Stool test came back clean 6 weeks later. I haven't had a twinge since. You got this. One pill at a time. 💪Radhika M December 26 2025
my mom took ppi for 5 years. then she broke hip. doctor said maybe ppi made bones weak. now she uses antacids only when needed. smart to not stay on it too long.