When you’re struggling to breathe, time matters. A tight chest, wheezing, or that gasping feeling after climbing stairs isn’t just uncomfortable-it’s scary. For millions with asthma or COPD, two types of inhalers are the difference between panic and peace: bronchodilators and corticosteroids. But they don’t work the same way, and using them wrong can make things worse.
What bronchodilators actually do
Bronchodilators are your quick fix. They don’t cure anything. They don’t reduce swelling. They simply make your airways wider-fast. Think of them like a door opener when everything’s jammed shut. There are two main types. The first are beta-2 agonists, like albuterol (also called salbutamol). These activate receptors in your airway muscles, telling them to relax. You feel the effect in 15 to 20 minutes. The relief lasts 4 to 6 hours for the short-acting versions, which is why they’re called SABAs. If you’ve ever carried a blue inhaler, that’s probably it. The second type is anticholinergics, like ipratropium or tiotropium. These block signals from your nervous system that cause airway tightening. They kick in about the same time as beta-2 agonists but last longer. Tiotropium, for example, works for a full 24 hours. That’s why it’s used daily in COPD. Long-acting bronchodilators (LABAs) like salmeterol or formoterol are designed for regular use, not emergencies. They take longer to start working-around 30 minutes-but keep airways open for 12 hours or more. But here’s the catch: using them alone without an anti-inflammatory drug increases your risk of a life-threatening asthma attack. That’s why they’re never prescribed by themselves for asthma.How corticosteroids work behind the scenes
Corticosteroids are the quiet heroes. You won’t feel them working right away. They don’t open your airways. They fix the root problem: inflammation. These aren’t the same as the anabolic steroids bodybuilders use. Inhaled corticosteroids like fluticasone, budesonide, and beclomethasone are designed to act locally in your lungs. They enter the cells lining your airways and switch off dozens of genes that cause swelling, mucus production, and sensitivity. It takes days-sometimes weeks-before you notice a difference. But over time, your lungs become less reactive. Fewer flare-ups. Fewer hospital visits. Studies show regular use cuts asthma exacerbations by 30% to 50%. For COPD patients with frequent flare-ups, this can mean the difference between staying home and ending up in the ER. But because they’re steroids, they come with side effects. The most common? Oral thrush-a fungal infection in the mouth that looks like white patches. It happens in 5% to 10% of users. The fix? Rinse your mouth with water and spit after every use. Don’t swallow it. That simple step cuts the risk in half. Another side effect is hoarseness or a sore throat. Again, rinsing helps. Some people also report a slight increase in pneumonia risk, especially older adults on high doses. That’s why doctors avoid pushing doses higher than needed.Why you need both-and how to use them right
Here’s where most people mess up. They use their corticosteroid inhaler first. Or they use it every time they feel short of breath. Or they don’t rinse. Or they don’t wait. The correct order is simple: bronchodilator first, wait five minutes, then corticosteroid. Why? Because inflamed, narrowed airways are like a closed door. You can’t get the corticosteroid deep into the lungs if the path is blocked. The bronchodilator opens the door. Then, the corticosteroid can reach where it’s needed. Studies show this sequence improves drug delivery by up to 40%. One patient on Reddit said, “I didn’t realize how much better my breathing was until I started waiting 5 minutes between inhalers-my Pulmocort actually works now.” That’s not luck. That’s science. And don’t skip the spacer. If you’re using a metered-dose inhaler (the kind that sprays), a spacer-a plastic tube attached to the mouthpiece-helps more medicine reach your lungs and less stick to your throat. Research shows it boosts effectiveness by 70%. Many people don’t even know they exist.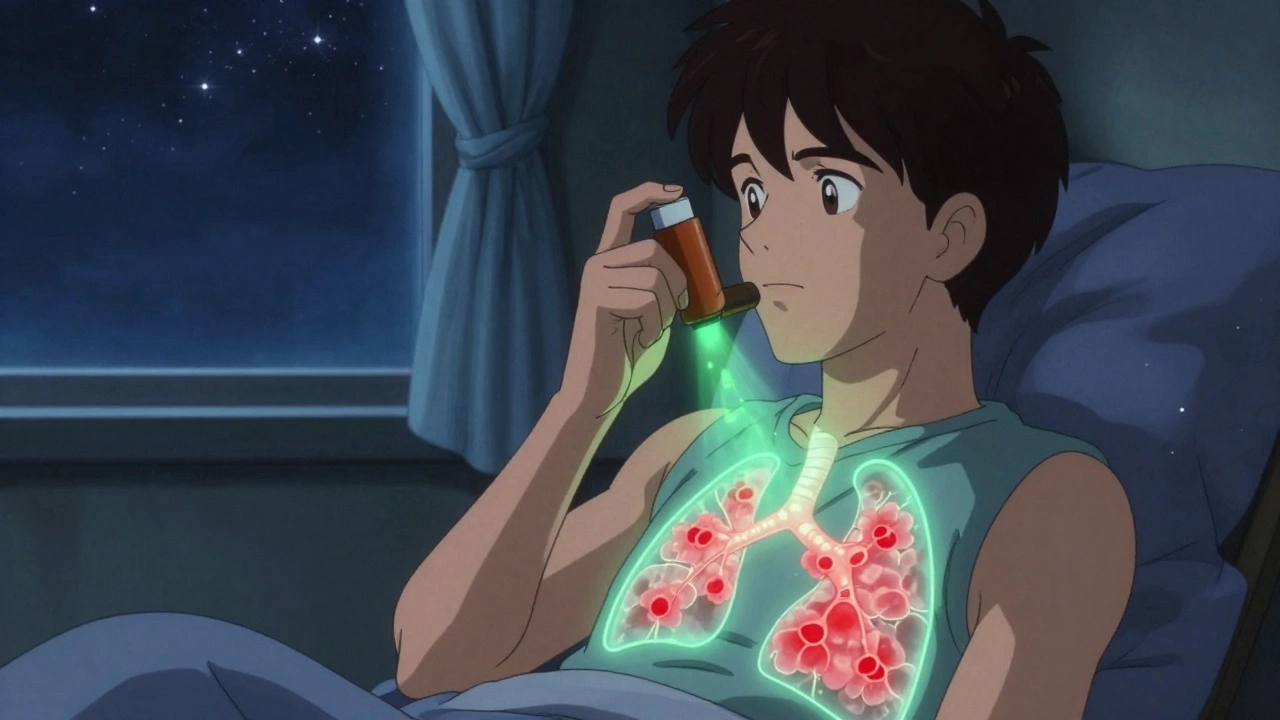
Combination inhalers: The new standard
Because using two inhalers correctly is hard, manufacturers made combination devices. Advair (fluticasone/salmeterol), Symbicort (budesonide/formoterol), and Breo Ellipta (fluticasone/vilanterol) all pack both drugs into one inhaler. These are now the most common prescription for moderate to severe asthma. In the U.S., 68% of asthma prescriptions are for combination inhalers. They simplify treatment and reduce errors. Even better, newer options like Airsupra (albuterol/budesonide) are designed for as-needed use. Instead of reaching for a blue rescue inhaler and a separate brown maintenance inhaler, you can use one device for both quick relief and anti-inflammatory action. The FDA approved it in 2023 based on trials showing it reduces severe flare-ups by 64% compared to using albuterol alone. GINA 2023 guidelines now recommend this approach for mild asthma too. No more daily corticosteroids unless needed. Just use the combo inhaler when symptoms appear.What patients get wrong-and how to fix it
You’d think this is straightforward. But data says otherwise. A 2022 American Lung Association survey found only 47% of patients could correctly identify which inhaler was for daily use and which was for emergencies. Forty-four percent couldn’t tell the difference. Common mistakes:- Using a rescue inhaler daily because they feel better afterward-this masks worsening inflammation.
- Not rinsing after corticosteroids, leading to thrush.
- Skipping the 5-minute wait between inhalers.
- Shaking the inhaler and spraying without inhaling deeply.
- Using old inhalers past their expiration date-some lose potency after 3 months.


Comments (14)
Annie Gardiner December 7 2025
Okay but have you ever tried breathing through a straw while someone sits on your chest? That’s what asthma feels like. And no, I don’t care if it’s ‘just inflammation’-when your lungs scream for air, you don’t care about science, you care about not dying.
Also, why is everyone acting like corticosteroids are some magical fairy dust? My mom got thrush so bad she couldn’t eat for a week. Rinsing doesn’t fix everything. Sometimes you just need to stop taking it.
And who decided 5 minutes between inhalers is the holy number? My pulmonologist said 2 minutes is fine if you’re gasping. Don’t turn medicine into a ritual.
Rashmi Gupta December 7 2025
People in India don’t even have access to inhalers. My cousin used to inhale steam from boiled neem leaves when she wheezed. No doctor. No spacer. No ‘combination inhalers.’
And now you’re telling me the ‘correct’ way is to wait five minutes? In a slum with no running water? You’re not helping. You’re just making people feel guilty for surviving.
Kumar Shubhranshu December 8 2025
Blue inhaler = emergency. Brown = daily. Rinsing = mandatory. Spacer = free. Done.Mayur Panchamia December 8 2025
America thinks it invented medicine! We’ve had Ayurvedic bronchodilators for 5000 years-turmeric, ginger, licorice root-and you’re telling me to use a $300 inhaler with a plastic tube? Pathetic! Your lungs are weak because you eat processed junk and sit on couches all day! We don’t need your fancy science-we need discipline!Kenny Pakade December 10 2025
This is why America is collapsing. People can’t even use an inhaler right. You need a PhD to breathe now? I’ve been using my blue inhaler since I was 12 and never rinsed. Still alive. Still breathing. Your ‘science’ is just corporate marketing dressed up as medical advice.Brooke Evers December 12 2025
I just want to say how much I appreciate this post. I’ve been living with COPD for 12 years and I never knew about the spacer thing until I saw a video on YouTube last year. My doctor never mentioned it. I thought the puffing was enough.
After I started using it, I went from needing rescue inhalers 4 times a day to maybe once a week. I cried when I realized how much I’d been suffering because no one told me how to use the damn thing properly.
If you’re reading this and you’re unsure-go to your pharmacy. Ask. Don’t be embarrassed. I was too. But my lungs are better now because I asked. And if you’re a caregiver-watch someone use their inhaler. You might save their life. You really might.
Saketh Sai Rachapudi December 13 2025
this is why indians are smarter than americans we dont need all this fancy stuff my grandad had asthma for 60 years and he used a pipe and tobacco smoke to open his lungs and he lived to 89. you people are too soft. why do you need a 300 dollar device when a cigarette works better? lolPriya Ranjan December 14 2025
Let me be clear: if you’re using a rescue inhaler more than twice a week, you’re not managing your condition-you’re ignoring it. And if you’re not rinsing after corticosteroids? You’re asking for thrush. It’s not a side effect-it’s negligence.
I’ve seen patients refuse to use spacers because they’re ‘too complicated.’ Then they show up in the ER with oxygen masks on. You don’t get to be lazy and then blame the medicine.
And yes, I’ve been a respiratory nurse for 22 years. I’ve watched people die because they thought ‘feeling fine’ meant ‘cured.’ It doesn’t. Inflammation doesn’t knock. It breaks down the door.
Gwyneth Agnes December 14 2025
Rinse. Wait. Spacer. Done.Ashish Vazirani December 16 2025
Let me tell you about my cousin. He had asthma. He used his inhaler. He didn’t rinse. He got thrush. He got pneumonia. He ended up in ICU for 17 days. His wife cried every night. His kids didn’t recognize him.
And when he got out? He still didn’t rinse. Said it ‘felt weird.’
He died last year. Age 41.
Don’t be him.
I’m not trying to scare you. I’m just saying-you have a choice. And your lungs? They don’t get a second chance.
Mansi Bansal December 17 2025
While I commend the article for its clinical accuracy, I must express profound concern regarding the sociopolitical implications of pharmaceutical commodification in respiratory care. The reliance on patented combination inhalers-many of which are manufactured by multinational corporations with opaque pricing structures-reinforces a neoliberal healthcare paradigm wherein patient autonomy is subordinated to corporate profit motives.
Furthermore, the normalization of spacer usage, while clinically sound, inadvertently stigmatizes those who cannot afford such adjunct devices. One wonders whether the GINA guidelines adequately account for global health inequities, or if they merely reflect the privileged Western clinical experience.
Is it ethical to recommend Airsupra as a first-line agent when its annual cost exceeds the GDP per capita of 147 nations? This is not medicine. This is market logic disguised as clinical guidance.
Katie O'Connell December 19 2025
While the article is technically accurate, it lacks a critical phenomenological dimension. The lived experience of dyspnea cannot be reduced to pharmacokinetic profiles or spacer efficacy percentages. The anxiety, the shame of wheezing in public, the silent panic during a Zoom meeting-these are the real metrics of disease burden.
And yet, the entire discourse remains anchored in biomedical reductionism. Where is the space for emotional labor? For grief? For the quiet mourning of a body that no longer obeys?
Perhaps what we need is not better inhalers, but better ways to sit with suffering-not fix it, just be with it.
Inna Borovik December 20 2025
Let’s be real-most people don’t even know what a metered-dose inhaler is. I’ve seen patients shake it like a soda can, spray it into the air, then take a deep breath like they’re inhaling perfume.
And don’t get me started on the ‘I feel fine so I skip it’ crowd. You think inflammation is a mood? It’s a silent killer. It’s the reason your grandma died at 72 from ‘complications’ after a cold.
Also, the carbon footprint point? Valid. But switching to dry powder inhalers won’t fix the fact that 80% of the world’s population can’t even get basic meds. This feels like rich people’s guilt dressed up as public health.
Andrew Frazier December 21 2025
I used to use my blue inhaler every day. Felt good. Then I got a new doc. Said I was abusing it. Told me to use the brown one instead. I did. Now I can run up stairs without feeling like I’m drowning. Why didn’t anyone tell me this before? My bad. But you know what? I’m not gonna feel guilty for being dumb. I’m just glad I figured it out.