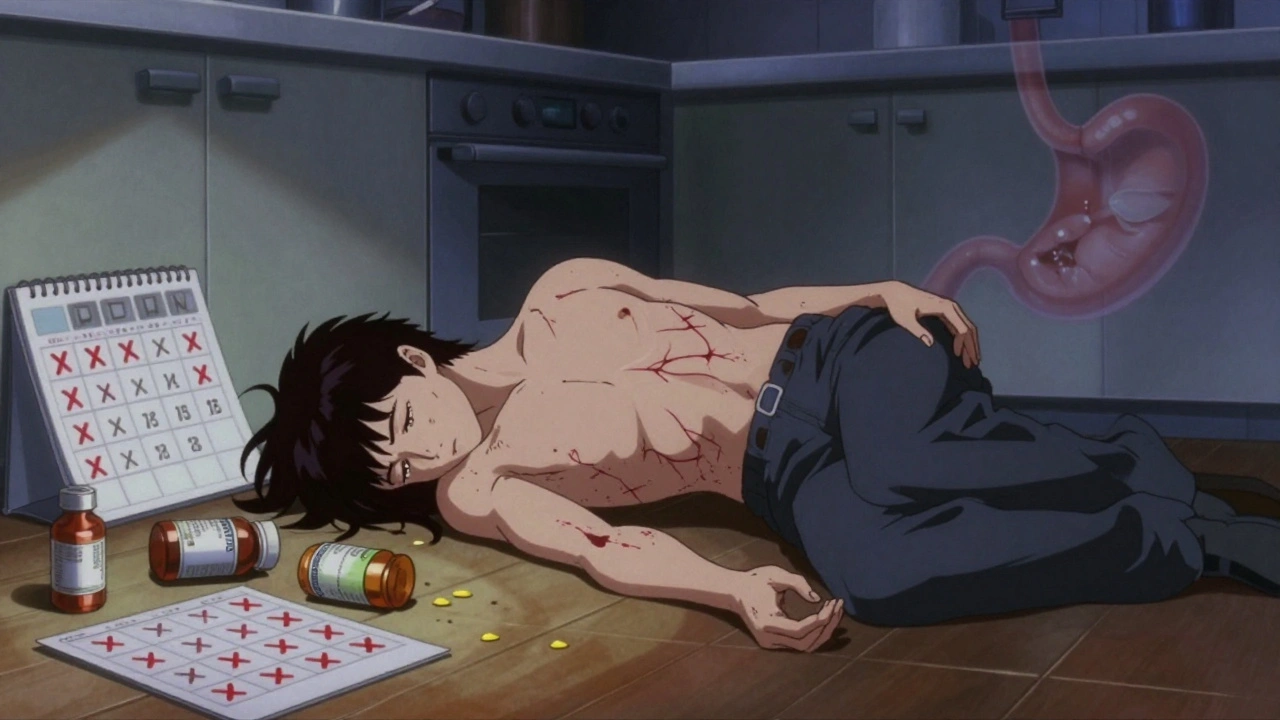
Every year, thousands of people end up in hospital because of something they thought was harmless: a daily painkiller. Not opioids. Not prescription sedatives. But NSAIDs - the very drugs you grab off the shelf for a headache, a sore back, or arthritic knees. What most don’t realize is that even taking the recommended dose, over time, can quietly damage your gut. And when it goes wrong, it doesn’t just hurt - it bleeds. Sometimes so badly, you don’t even notice until you’re fainting on the kitchen floor.
How NSAIDs Turn Your Gut Into a Slow Leak
NSAIDs - like ibuprofen, naproxen, diclofenac, and even low-dose aspirin - work by blocking enzymes called COX-1 and COX-2. These enzymes help make prostaglandins, chemicals your body uses to signal pain and inflammation. But they also help protect your stomach lining and keep blood flowing properly in your intestines. When you block COX-1, you’re not just turning down the pain - you’re turning off your body’s natural defense system against stomach acid. This isn’t just about heartburn. The damage happens deep inside your digestive tract. Studies show up to 70% of people who take NSAIDs long-term have visible damage in their stomach or intestines - erosions, ulcers, tiny bursts of bleeding - even if they feel fine. That’s the scary part. You can be bleeding internally for weeks and never know it. No burning. No nausea. Just fatigue, pale skin, or shortness of breath from iron-deficiency anemia.Who’s Most at Risk? It’s Not Who You Think
Most people assume only heavy users or the elderly are in danger. But the real danger zone is a mix of factors that stack up silently:- People on low-dose aspirin for heart protection - This is the most dangerous combo. Aspirin alone increases GI bleeding risk 2 to 4 times. Add another NSAID? That risk jumps 2 to 4 times again. One study found over one-third of people admitted for GI bleeding were taking over-the-counter aspirin daily - often without telling their doctor.
- Those with a past ulcer or bleeding episode - If you’ve had one GI bleed from NSAIDs before, your chance of another is extremely high. It’s not a one-time mistake - it’s a pattern.
- People with H. pylori infection - This common stomach bacteria doesn’t cause problems for most. But if you’re also taking NSAIDs, your bleeding risk goes up by 20%. Treat the infection first. Don’t just keep popping pills.
- Anyone on blood thinners or dual antiplatelet therapy - If you’ve had a heart attack and are on two anti-clotting drugs, adding NSAIDs can double your risk of dangerous bleeding. Doctors know this. Too many patients don’t.
- Older adults on multiple meds - The older you are, the more your stomach lining thins. Combine that with five or six other drugs, and your gut becomes a minefield.
The Myth of ‘Safe’ NSAIDs
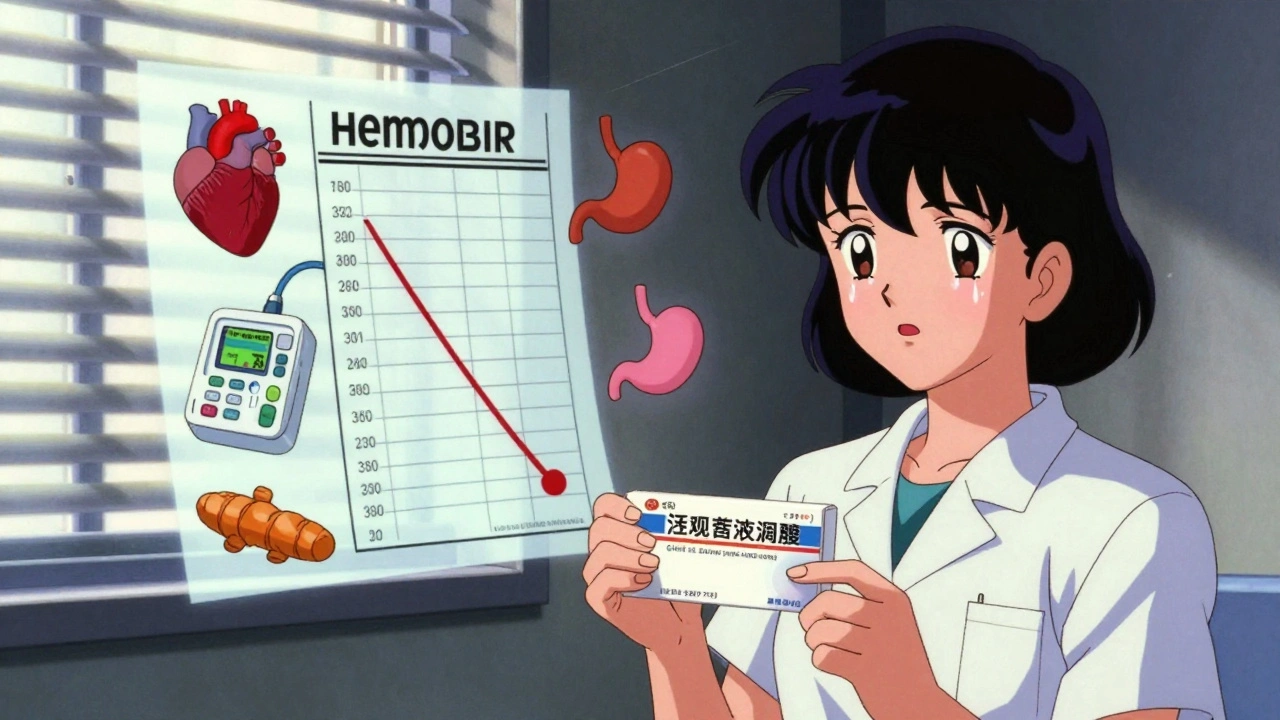
You’ve probably heard that “COX-2 inhibitors” like celecoxib are safer for your stomach. That used to be true - but only if you weren’t also taking aspirin. When you mix them, the protection disappears. One major study showed that people on both low-dose aspirin and a COX-2 inhibitor had a 7.5% chance of a serious upper GI event each year - worse than those on regular NSAIDs. That’s not safer. That’s a trap. And what about enteric-coated or buffered aspirin? They sound gentler. They’re not. They don’t reduce bleeding risk at all. The coating just delays the pill dissolving - it doesn’t stop the damage to your gut lining. The same goes for “low-dose” claims. Even 75mg of aspirin daily raises your bleeding risk. At 300mg? Your risk nearly quadruples.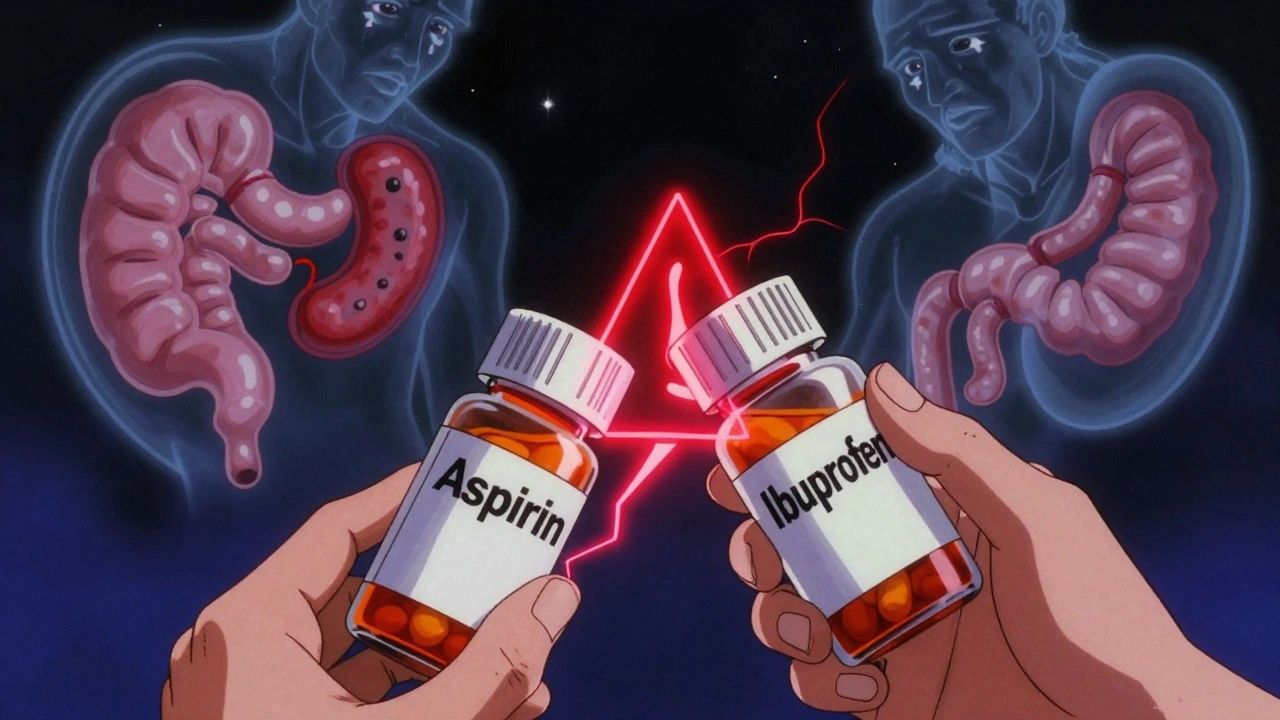
Why Symptoms Lie - and How to Catch the Real Signs
Dyspepsia - that burning, bloated feeling - is the most common complaint. But here’s the truth: if you have it, you might have an ulcer. If you don’t have it, you might still be bleeding. In clinical trials, over half of patients who became anemic from NSAID use showed no signs of bleeding on endoscopy. Their stomach looked fine. But they were losing blood slowly, day after day. The real red flags aren’t pain. They’re:- Unexplained tiredness or dizziness - especially if it’s new
- Pale skin or cold hands
- Shortness of breath during light activity
- Dark, tarry stools (melena)
- Red or bloody stools - though this is rarer and often means lower GI damage
- Iron deficiency anemia with no other cause
What to Do If You’re Already Taking NSAIDs
If you’re on NSAIDs - especially daily - here’s what you need to do right now:- Ask your doctor: Do I really need this? Many people take NSAIDs for minor aches that don’t need them. Physical therapy, heat, or acetaminophen might be enough.
- If you’re on aspirin for heart protection, don’t add another NSAID. Ever. If you need pain relief, talk to your doctor about alternatives. Acetaminophen is usually safer. If you must use an NSAID, limit it to the lowest dose for the shortest time.
- Get tested for H. pylori. If you’ve had a stomach ulcer before, or you’re over 60 and on NSAIDs, ask for a breath or stool test. Treating it cuts your bleeding risk significantly.
- Don’t assume PPIs fix everything. Proton pump inhibitors (like omeprazole) help protect your stomach. But they don’t stop bleeding in the small or large intestine. They’re helpful - but not a magic shield.
- Check your iron levels yearly. If you’re on long-term NSAIDs, ask for a ferritin test. Low iron doesn’t always mean you’re bleeding - but if it’s dropping, it’s a warning.
When to Stop NSAIDs Immediately
There’s no gray area here. If you’re on dual antiplatelet therapy - say, after a stent or heart attack - NSAIDs are a hard no. Studies show combining them with drugs like clopidogrel or ticagrelor increases GI bleeding risk two-fold and also raises your chance of heart attack or stroke. The risk isn’t just in your gut. It’s in your heart too. Same goes if you’ve had a previous GI bleed. Continuing NSAIDs after that is like walking back into a burning house. The chance of another bleed is so high, most guidelines say: stop them completely. Find another way to manage pain.What’s the Alternative?
You don’t have to live in pain. But you do have to rethink your options:- Acetaminophen (paracetamol) - Still the safest choice for most people on NSAID risk. Don’t exceed 4,000mg a day, and avoid if you have liver disease.
- Topical NSAIDs - Gels and patches deliver the drug right to the sore joint. Much less risk to your gut. Great for knee or shoulder pain.
- Physical therapy and movement - Often more effective long-term than pills. Especially for back and arthritis pain.
- Heat, cold, or TENS units - Simple, cheap, and safe. No drugs needed.
- Weight management - Losing even 5% of body weight can cut arthritis pain by half. That’s more powerful than any pill.
The Bottom Line: It’s Preventable
NSAID-related GI bleeding isn’t a rare accident. It’s a predictable consequence of widespread, unchecked use. Millions take these drugs without knowing the risk. Doctors prescribe them without always checking the full picture. And patients assume because it’s over-the-counter, it’s safe. It’s not. The truth is, your stomach doesn’t care if the pill was bought with a prescription or from a pharmacy shelf. It only cares about the chemistry. And NSAIDs, even in small doses, are designed to weaken your gut’s defenses. The fix isn’t complicated. It’s simple: Question every NSAID you take. Ask why. Ask how long. Ask if there’s a safer way. Get tested. Check your blood. Talk to your doctor - not just when you’re in pain, but before you start taking anything regularly. Because the next time you reach for that bottle of ibuprofen, you might not just be relieving pain. You might be setting a timer.Can I take aspirin and ibuprofen together?
No. Combining low-dose aspirin (used for heart protection) with ibuprofen or other NSAIDs increases your risk of gastrointestinal bleeding by 2 to 4 times. Even if you take them hours apart, ibuprofen can block aspirin’s protective effect on the heart. If you need pain relief while on aspirin, use acetaminophen instead. Always check with your doctor before mixing any painkillers.
Do PPIs completely prevent NSAID-related bleeding?
No. Proton pump inhibitors (PPIs) like omeprazole help protect your stomach lining and reduce the risk of upper GI ulcers and bleeding. But they don’t stop damage in the small or large intestine, where NSAIDs can still cause silent bleeding and inflammation. Studies show over half of NSAID users who become anemic show no visible lesions on endoscopy - meaning PPIs aren’t a full shield. They help, but they’re not enough on their own.
I feel fine taking NSAIDs daily. Why should I stop?
Feeling fine doesn’t mean you’re not being damaged. Up to 70% of long-term NSAID users show visible gut injury on endoscopy - even if they have zero symptoms. Bleeding can be slow and hidden, causing iron deficiency anemia without warning. Fatigue, dizziness, or pale skin might be the only signs. By the time you feel pain, the damage may already be serious. Regular blood tests and a doctor’s review are essential if you’re on NSAIDs long-term.
Is it safe to take NSAIDs occasionally, like once a week?
For most healthy adults, occasional use - like once or twice a week for a headache or sprain - carries very low risk. But if you’re over 65, have a history of ulcers, take blood thinners, or have kidney or heart disease, even occasional use can be dangerous. The key isn’t frequency - it’s your personal risk profile. If you’re unsure, talk to your doctor before taking any NSAID, even infrequently.
Can I switch to a natural remedy instead of NSAIDs?
Some natural options like turmeric, ginger, or omega-3s have mild anti-inflammatory effects and may help with chronic pain - especially arthritis. But they’re not strong enough to replace NSAIDs for acute or severe pain. They also aren’t risk-free. Turmeric can thin blood, and fish oil can interact with anticoagulants. Never assume “natural” means safe. Always discuss supplements with your doctor, especially if you’re on other medications.
What’s the safest NSAID for my stomach?
There’s no truly safe NSAID when it comes to your gut. Even COX-2 inhibitors like celecoxib, once thought to be gentler, offer no protection if you’re also taking aspirin. All NSAIDs carry some level of GI risk. The safest approach isn’t choosing a “better” NSAID - it’s using the lowest effective dose for the shortest time, and only when necessary. For most people, acetaminophen or non-drug options are better first choices.

Comments (12)
Victoria Graci December 1 2025
It’s wild how we’ve turned medicine into a vending machine culture-pop a pill, forget the body’s whispering SOS. NSAIDs don’t just ‘irritate’ the gut-they dismantle its ancient, elegant defenses like a toddler with a blowtorch. The stomach didn’t evolve to handle daily chemical sabotage. It evolved to digest, not to endure pharmaceutical neglect. And yet we treat it like a disposable filter. The real tragedy? The body doesn’t scream until it’s collapsing. By then, it’s too late for ‘maybe I should’ve listened.’
Chelsea Moore December 2 2025
THIS IS WHY WE CAN’T HAVE NICE THINGS!!! 🚨 I’ve been saying this for YEARS!! People think ‘over-the-counter’ means ‘safe for your soul’-NOPE. It means ‘profitable for Big Pharma’ and ‘disposable for your intestines’!! I had a cousin bleed out from ibuprofen and they didn’t even know they were at risk!! WHY DO WE LET THIS HAPPEN??
Anthony Breakspear December 2 2025
Man, I used to pop two Advil after every workout like it was candy. Then I got dizzy one morning, looked in the mirror, and my face was the color of printer paper. Turns out my ferritin was in the basement. Doc said, ‘You’ve been bleeding silently for 11 months.’ I thought I was just ‘getting old.’ Turns out I was just stupid. Now I use heat packs, stretch like a yoga zombie, and if I need pain relief? Tylenol. No drama. No drama at all.
Genesis Rubi December 3 2025
Why are we even talking about this? In America we have the best healthcare in the world-why are people still dying from dumb mistakes? If you can’t read a label, maybe you shouldn’t be allowed to buy pills. I mean, come on. This isn’t rocket science. It’s a bottle. With words. On it.
Allan maniero December 4 2025
There’s something quietly heartbreaking about how we’ve normalized self-medication as a lifestyle. We treat pain like a glitch to be silenced, not a signal to be understood. The irony? The body’s been whispering for millennia-pain, fatigue, pallor-and we’ve trained ourselves to deafen it with chemical noise. Maybe the real crisis isn’t NSAIDs-it’s our collective refusal to sit still long enough to listen.
Eddy Kimani December 5 2025
COX-1 inhibition = reduced prostaglandin E2 → decreased mucosal blood flow + diminished bicarbonate secretion → loss of gastric barrier integrity. That’s the molecular cascade. But clinically? It’s silent hemorrhage masked as ‘fatigue.’ Most patients don’t present with melena until Hgb drops below 7. That’s why ferritin screening is non-negotiable for chronic NSAID users. Also, PPIs only protect the stomach-duodenum and jejunum? Still vulnerable. Need to think regionally, not just topographically.
Doug Hawk December 5 2025
i took naproxen for my back for like 3 years and never felt anything wrong until one day i passed out in the shower. turns out my hgb was 5.8. doc said if i had waited another week i wouldve needed a transfusion. now i do yoga and ice packs. also i never take anything without asking my pharmacist first. they know more than you thinkSaravanan Sathyanandha December 7 2025
In India, we have a phrase: ‘Dard kam, zindagi zyada’-less pain, more life. But modern medicine often reverses this. We treat symptoms like enemies, not messengers. NSAIDs are not villains-they’re tools. But tools without wisdom become weapons. I’ve seen grandmothers in villages manage arthritis with turmeric paste, warm oil massages, and walking barefoot on dew-covered grass. Not because they’re poor-but because they remember the body speaks in rhythm, not in pills. Maybe we need to unlearn, not just prescribe.
Sandi Allen December 7 2025
THIS IS A LIBERAL SCAM TO MAKE PEOPLE FEEL GUILTY FOR TAKING PAINKILLERS!!!!!! WHO DO YOU THINK YOU ARE, TELLING ME WHAT TO DO WITH MY BODY??!!! I’M A FREE AMERICAN!!! I’LL TAKE IBUPROFEN WITH MY COFFEE, MY BREAKFAST, AND MY EVENING NEWS!!!!!! IF I BLEED, IT’S MY BUSINESS!!!!!! YOU’RE JUST A MEDICAL ELITIST WHO WANTS TO CONTROL EVERYTHING!!!!!! THE GOVERNMENT ISN’T TELLING ME WHAT TO DO!!!!!!
John Biesecker December 9 2025
lol i just realized i’ve been taking aspirin daily since 2018 for my ‘heart’ and ibuprofen every friday for my knees 😅 i’m gonna go ask my doc if i’m basically a walking time bomb 🤣 maybe i’ll start drinking more water and doing squats instead? 🤔Elizabeth Farrell December 10 2025
I’ve been a nurse for 18 years, and I’ve held the hands of too many people who didn’t realize their fatigue was their body screaming for help. One woman came in with a hemoglobin of 4.2-she thought she was just ‘tired from work.’ She’d been taking OTC naproxen for her arthritis for 7 years. She didn’t even know it was connected. I wish every person who reaches for a painkiller would pause for 10 seconds and ask: ‘Is this helping me… or just hiding the problem?’ You deserve to live without pain, yes-but you also deserve to live without silently destroying yourself.
Fern Marder December 10 2025
Okay but like… I’m 32 and I take 2 ibuprofen every time I get my period. Is that a problem? 😅 I mean, I feel fine. But now I’m paranoid. Should I be getting blood work? Should I just… stop? 🥺 I don’t want to be one of those people who ends up in the ER with no warning. Also, can I just use a heating pad forever? 🫠