Lactic Acidosis Risk Assessment Tool
Assess Your Risk
This tool helps identify potential risk factors for medication-induced lactic acidosis based on information from the article.
Important Notes
This tool is for informational purposes only and doesn't replace medical advice. Always consult your doctor.
Critical information from the article:
lactate levels above 4 mmol/L and pH below 7.35 indicate dangerous acidosis
Remember: Lactic acidosis often has vague symptoms like fatigue and rapid breathing. Don't ignore these signs, especially when taking high-risk medications.
Your Risk Assessment
Key Risk Factors Identified
Recommended actions:
Most people think of medication side effects as nausea, dizziness, or a rash. But there’s a silent, deadly reaction hiding in plain sight: lactic acidosis. It doesn’t show up on a routine blood test. It doesn’t always cause obvious symptoms. And by the time it’s caught, it’s often too late. This isn’t a theoretical risk. It’s a real, documented danger tied to common drugs-drugs millions of people take every day.
What Exactly Is Lactic Acidosis?
Lactic acidosis happens when your body makes too much lactic acid and can’t clear it fast enough. Normal lactate levels are between 0.5 and 2.2 mmol/L. When they climb above 4-5 mmol/L-and your blood pH drops below 7.35-you’re in danger. This isn’t just a lab abnormality. It’s a metabolic crisis. Your cells are starved of oxygen at the mitochondrial level, and your body is forced to burn sugar without oxygen, flooding your bloodstream with acid.
Unlike lactic acidosis from shock or heart failure (Type A), the kind caused by medications is Type B. That means your tissues aren’t dying from lack of blood flow. Something in the drug itself is breaking your energy production. And that’s what makes it tricky. You might be stable, breathing fine, with good blood pressure-and still be slipping into acidosis because a pill you took yesterday is quietly sabotaging your mitochondria.
Drugs That Can Trigger It (And How)
Over 50 medications have been linked to lactic acidosis. Some are obvious risks. Others? You’d never guess.
- Metformin: The most common culprit among diabetes drugs. Used by over 150 million people worldwide. It doesn’t cause lactic acidosis on its own. It needs a trigger-like kidney trouble, infection, or dehydration. In patients with eGFR under 60 mL/min, risk jumps. The fatality rate? Around 22%. That’s why it carries a black box warning. But many doctors still prescribe it in mild kidney disease, assuming it’s safe. It’s not always.
- Linezolid: An antibiotic for tough infections like MRSA. It blocks mitochondrial protein production. After 14 days of use, the risk spikes. One study found 15% of patients on long-term linezolid developed elevated lactate. Many never made it to the hospital before crashing.
- Albuterol: The go-to inhaler for asthma attacks. Sounds harmless, right? Wrong. It overstimulates your muscles, forcing them to burn sugar like crazy. At the same time, it shuts down the enzyme that turns pyruvate into energy. Result? Lactate piles up. One case showed lactate hitting 11 mmol/L after standard nebulizer treatment-dropping to 4.5 mmol/L after cutting back. Doctors often mistake the rapid breathing from acidosis for worsening asthma-and give more albuterol. A deadly loop.
- Propofol: Used in ICUs for sedation. High doses over 48 hours can trigger Propofol Infusion Syndrome. Lactic acidosis is one of its hallmarks. Mortality? Over 66%. It’s rare, but when it hits, it’s brutal.
- Acetaminophen: Even at normal doses, it can cause lactic acidosis in older adults with liver or kidney issues. Symptoms? Confusion, fatigue, fast breathing. Often dismissed as "just getting older." Diagnosis delays average 36 hours. That’s time the body loses.
- NRTIs (HIV drugs): These drugs damage mitochondrial DNA. Women, people with low CD4 counts, and those with poor kidney function are at highest risk. A 2023 study found a gene variant (POLG) that makes someone 8 times more likely to develop it.
Who’s Most at Risk?
It’s not random. Certain people are sitting ducks.
- People over 65
- Those with kidney disease (eGFR under 60)
- Patients with liver cirrhosis
- Anyone with sepsis or severe infection
- People on multiple high-risk drugs at once
- Women taking NRTIs
One review found 72% of metformin-related lactic acidosis cases involved kidney impairment. Another found the median age of victims was 68. These aren’t outliers. They’re predictable.
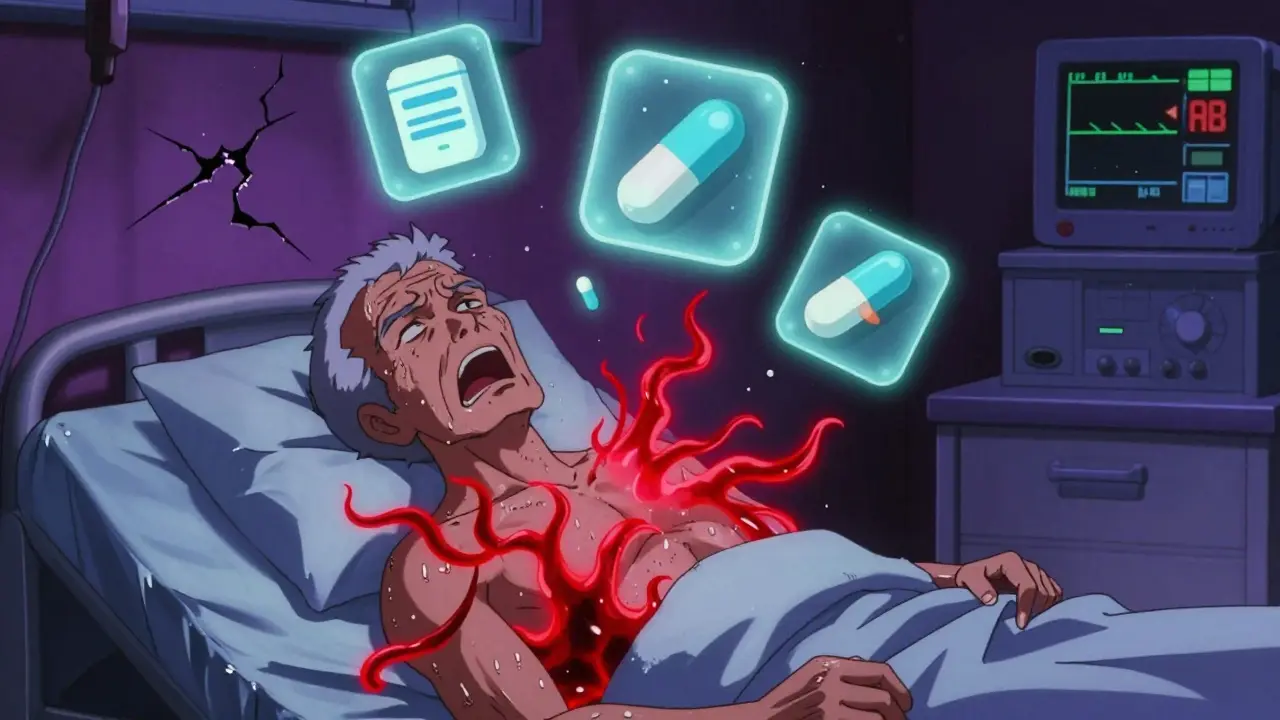
Why Is It So Often Missed?
Because it looks like something else.
In the ICU, a patient’s lactate is high. Is it sepsis? Heart failure? The drug? Doctors are trained to look for the big, obvious causes. Medications? They’re assumed to be safe. A 2019 review found that in over 40% of cases, the offending drug was never stopped-even when lactate was sky-high.
And here’s the kicker: many clinicians don’t even check lactate unless the patient is crashing. But by then, it’s often too late. Lactic acidosis creeps up. It starts with fatigue. Then nausea. Then faster breathing. Then confusion. Then low blood pressure. Then organ failure. The symptoms are vague. The progression is slow. Until it isn’t.
One pulmonologist on a medical forum summed it up: "I’ve seen multiple cases where we kept escalating albuterol for worsening respiratory status without realizing the nebs were causing the metabolic acidosis that was driving the tachypnea."
How Is It Diagnosed and Treated?
Diagnosis is simple: check the lactate. If it’s above 4 mmol/L and the blood pH is under 7.35, you’ve got it. But many hospitals don’t routinely test lactate unless the patient is in shock. That’s the problem.
Treatment? Stop the drug. Immediately. Unless it’s life-saving-like epinephrine in anaphylaxis. Then you manage the acidosis while keeping the drug going.
- Give IV fluids: 20-30 mL/kg to flush out the acid and improve circulation.
- For metformin: if lactate is over 20 mmol/L or pH under 7.1, start hemodialysis. It removes both metformin and lactate.
- For linezolid or NRTIs: stop the drug. Supportive care. Lactate usually drops within 24-48 hours.
- Bicarbonate? Controversial. Most guidelines say don’t use it unless pH is below 7.15. It doesn’t save lives-it just masks the problem.
Monitoring matters. Lactate should drop by 50% within two hours of stopping the drug and starting fluids. If it doesn’t, look for another cause-or another drug.
What’s New in Prevention?
There’s progress.
In 2023, the FDA approved a new device called Lactate Scout+. It’s a handheld monitor that gives real-time lactate readings. Early results show it cuts detection time from over 12 hours to just over 2 hours. That’s huge.
The 2024 International Critical Care Guidelines now recommend routine lactate checks for anyone on continuous epinephrine or high-dose beta-agonists. That’s a game-changer.
Researchers are also looking at genetic testing. If you have the POLG gene variant, you shouldn’t take certain HIV drugs. Simple blood test. Big impact.
And for metformin? The rules changed in 2016. It’s now considered safe in mild kidney disease (eGFR 45-59) if monitored closely. But many doctors still avoid it entirely. That’s overcautious. The real risk is in ignoring kidney function altogether.
What Should You Do?
If you’re on one of these drugs:
- Know your kidney function. Ask for your eGFR number. If it’s under 60, talk to your doctor about alternatives.
- Don’t ignore fatigue, nausea, or rapid breathing-especially if you’re on albuterol or metformin.
- If you’re hospitalized and on linezolid for more than 10 days, ask if lactate has been checked.
- If you’re on multiple medications, especially in the ICU, make sure someone is tracking lactate levels.
- Never assume a drug is "safe" just because it’s common.
Doctors aren’t ignoring this. But they’re overwhelmed. Patients have to be their own advocates. If you feel off-really off-ask: "Could this be lactic acidosis?"
It’s rare. But it’s real. And it kills.
Can metformin cause lactic acidosis even if my kidneys are fine?
Yes, but it’s rare. Metformin alone rarely causes lactic acidosis. It usually needs a trigger-like a severe infection, heart failure, dehydration, or liver disease. Even with normal kidney function, if you’re critically ill, your body can’t clear lactate properly. That’s why doctors check for other conditions before assuming metformin is the cause.
Is lactic acidosis from albuterol common?
It’s not common in the general population, but it’s underrecognized. In emergency rooms and ICUs, albuterol is one of the top 3 drugs linked to lactic acidosis. Patients with asthma or COPD often get repeated nebulizer treatments. Each dose pushes lactate higher. If they’re already dehydrated or have poor lung function, the acidosis can build fast. Many clinicians don’t connect the dots until the patient crashes.
How long does it take for lactate to drop after stopping the drug?
In most medication-induced cases, lactate should drop by at least 50% within 2 hours of stopping the drug and giving IV fluids. If it doesn’t, something else is going on-like ongoing infection, liver failure, or another drug. A slow drop means the problem isn’t just the medication.
Can I get tested for genetic risk before taking NRTIs?
Yes, but it’s not routine yet. A 2023 study found a specific variant in the POLG gene increases the risk of NRTI-induced lactic acidosis by over 8 times. Testing exists, but it’s mostly used in research or high-risk cases. If you’re on HIV meds and have unexplained fatigue or muscle pain, ask your doctor about genetic screening.
Should I stop my medication if my lactate is high?
Usually, yes-if it’s safe to do so. For drugs like metformin, linezolid, or albuterol, stopping them is the first step. But if you’re on epinephrine for shock or insulin for diabetic ketoacidosis, stopping could kill you. In those cases, you treat the acidosis while keeping the drug going. Always consult your doctor. Never stop a critical medication on your own.

Comments (14)
steve rumsford January 7 2026
man i never thought albuterol could do this. i’ve been on nebs for years and now i’m side-eyeing my inhaler like it’s a secret villain.
Emma Addison Thomas January 8 2026
Interesting read. I’ve seen elderly patients in the UK with mild renal impairment still on metformin, and the assumption is always ‘it’s fine.’ But this makes me wonder how many silent cases we’re missing.
Christine Joy Chicano January 9 2026
This is the kind of post that should be mandatory reading for every med student. Lactic acidosis isn’t some rare footnote-it’s a slow-motion bomb disguised as a routine prescription. And the fact that doctors often miss it because it ‘looks like’ something else? That’s systemic negligence wrapped in white coats.
Propofol in the ICU? Linezolid for stubborn MRSA? Albuterol in asthma exacerbations? These aren’t ‘edge cases’-they’re everyday tools. And we’re treating them like candy.
It’s not about fear. It’s about awareness. We need lactate checks on anyone on these meds longer than 48 hours, not just when they’re gasping on the floor.
And that Lactate Scout+? Finally. A tool that doesn’t wait for collapse to scream ‘DANGER.’
Why isn’t this in every ER protocol? Why does it take a patient crashing to trigger a test? We’re still playing whack-a-mole with medicine instead of installing smoke detectors.
Someone needs to write a patient pamphlet on this. Not a 10-page journal article. A plain-English flyer you can stick on your fridge next to your insulin log.
And yes, I’m ranting. Because I’ve seen it. And I’m tired of hearing ‘it’s rare.’ Rare doesn’t mean ‘not worth caring about.’ It means ‘you’re lucky it hasn’t hit you yet.’
Paul Mason January 10 2026
Look, I get it, metformin’s got a black box warning, but people are terrified of it for no reason. If your kidneys are even a little off, sure, swap it. But if you’re 55 and healthy with an eGFR of 58? You’re fine. Stop being paranoid.
Also, acetaminophen? Come on. That’s like saying water can drown you. Sure, if you drink a bathtub full, but nobody’s doing that.
Stop scaring people with rare edge cases. We’re not all going to drop dead from a pill.
Anastasia Novak January 11 2026
Oh wow. So the pharmaceutical industry is quietly poisoning people through ‘safe’ meds and nobody’s suing anyone? Shocking. Of course the FDA approves this. They’re paid off. Of course doctors ignore it. They’re in the pocket of Big Pharma. Of course you need to test your own lactate-because the system is designed to kill you slowly.
They’ll tell you it’s ‘rare’ until your kidneys fail and your blood turns to vinegar. Then they’ll say ‘we didn’t know.’
And that ‘new device’? Just another way to make you pay more. You’ll need a subscription to Lactate Scout+ just to stay alive. Classic.
Poppy Newman January 12 2026
Wow. This changed my perspective 😳 I’m on metformin and my eGFR is 57… I’m calling my doctor tomorrow. Thank you for posting this. 🙏
Mina Murray January 14 2026
They don’t want you to know this. Metformin was originally derived from French lilac-a plant that lowers blood sugar but also causes lactic acidosis. They ‘refined’ it, made it ‘safe,’ but kept the killer mechanism. Why? Because diabetes is a cash cow. Millions of people on lifelong meds. Who cares if 0.2% die? It’s still profitable.
And the FDA? They’re not regulators. They’re corporate lobbyists with badges. You think they’d approve a drug that kills 1 in 500 users if it made billions? Of course they would. They did.
Check your meds. Cross-reference every pill you take with the FDA’s adverse event database. You’ll be shocked. And then you’ll be scared.
Jessie Ann Lambrecht January 15 2026
This is such an important wake-up call. I work in a clinic and I’ve had patients come in with fatigue and rapid breathing-told them it was ‘just stress’ or ‘old age.’ Now I’m kicking myself. I’m going to start checking lactate in anyone over 60 on metformin or albuterol, even if they seem fine.
And yes, bicarbonate is a bandaid. We treat the symptom, not the cause. We need to stop that.
Thank you for writing this. I’m sharing it with every nurse and PA I know.
LALITA KUDIYA January 16 2026
this is eye opening i never knew albuterol could do this 😮Andrew N January 17 2026
Let’s be real-this is just another fearmongering article. Lactic acidosis from meds? Yeah, it happens. But so does death from eating too much salt. That doesn’t mean we ban table salt.
If you’re on metformin and your kidneys are fine, you’re fine. Stop reading alarmist blogs and start trusting your doctor.
Also, why are we even talking about this? Nobody’s dying from this. It’s statistically irrelevant.
Adam Gainski January 17 2026
Great breakdown. I’m a nurse and I’ve seen this happen twice-both times, the drug was never suspected until the patient was coding.
One was on linezolid for osteomyelitis, 18 days in. Lactate was 12.5. They were ‘just tired.’ Another was on albuterol for COPD, got 6 nebs in 2 hours, lactate hit 9.8. They thought it was ‘worsening disease.’
What we need isn’t more awareness-it’s protocol. Lactate check at 24h for anyone on linezolid, propofol, or high-dose beta-agonists. Simple. Mandatory.
And for patients: if you’re on metformin and feel like you’ve been hit by a truck after a meal, don’t brush it off. Get a lactate test. It takes 5 minutes. Could save your life.
Kamlesh Chauhan January 19 2026
why is everyone so scared of pills?? just stop taking them if u r scared lolKatrina Morris January 20 2026
I’m so glad someone finally wrote this. My mom was on metformin and got really sick after a UTI-doctors thought it was just the infection. Turns out her lactate was 8.2. She almost didn’t make it.
She’s fine now, but we never knew to check. I’m telling everyone I know. This isn’t scary-it’s just not taught enough.
Thank you for making it clear. I’ll be asking my doctor for a lactate test next time I get bloodwork.
Anthony Capunong January 20 2026
Look, I don’t care what some blog says. In America, we trust our doctors. If they prescribe it, it’s safe. You think they’d let a killer drug on the market? That’s a European conspiracy theory.
Metformin’s been around for 60 years. Millions of Americans use it. If it was dangerous, we’d know. We’re not guinea pigs.
Stop scaring people with foreign studies and fear-mongering. We have the best healthcare system in the world.