Eye Inflammation Assessment Tool
Eye Inflammation Assessment
This tool helps you assess if you might be experiencing eye inflammation based on your symptoms and risk factors. Remember: This is not a substitute for professional medical advice. Always consult an eye doctor for proper diagnosis.
Your Assessment
Quick Takeaways
- Early detection of eye inflammation can prevent permanent vision loss.
- Uveitis, conjunctivitis, and keratitis are the most common inflammatory eye conditions.
- Inflammation can raise intraocular pressure, damage the retina, and trigger cataract formation.
- Systemic diseases like autoimmune disorders and diabetes increase the risk of ocular inflammation.
- Treatment ranges from topical antibiotics to systemic immunosuppressants, depending on severity.
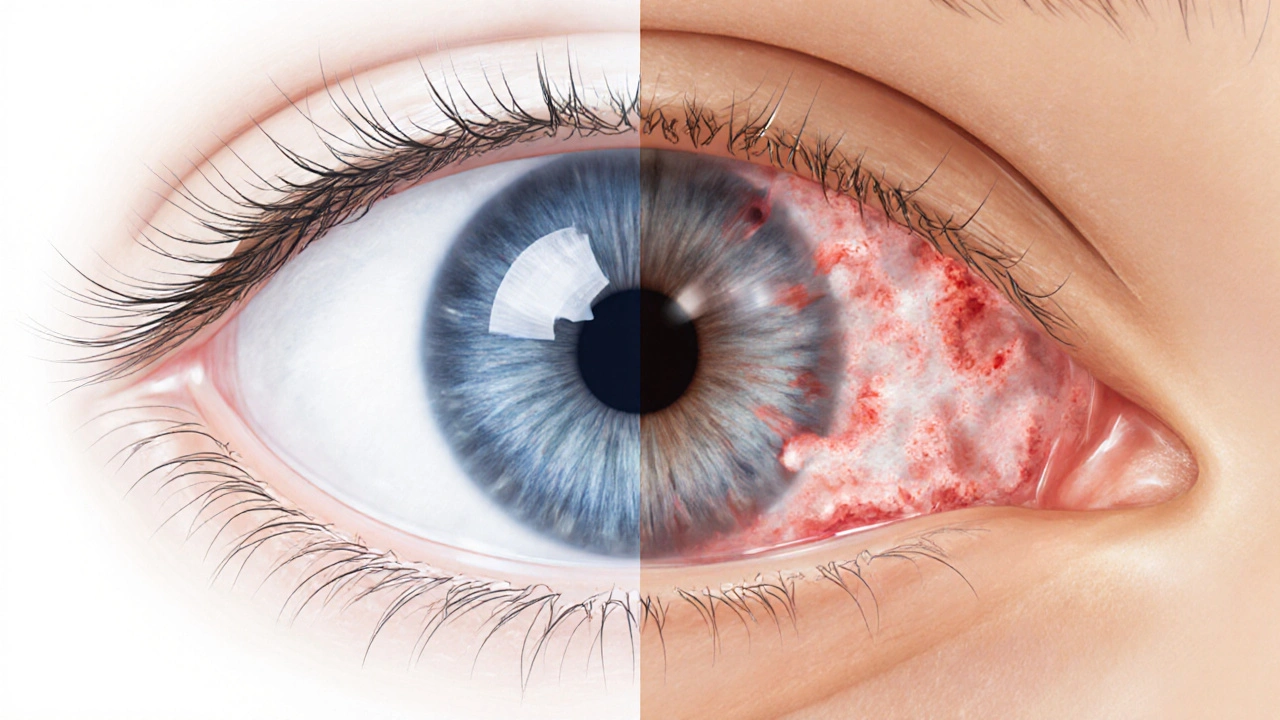
What Is Eye Inflammation?
Eye inflammation is a broad term for any swelling, redness, or irritation affecting the structures of the eye. It can involve the outer surface (conjunctiva), the cornea, the iris, the uveal tract, or even the retina. The inflammatory response is meant to protect the eye from infection or injury, but when it becomes chronic or severe, it starts to damage delicate tissue and impair visual function.
Common Types of Ocular Inflammation
Three conditions account for the majority of eye‑related inflammation cases:
- Uveitis: Inflammation of the uveal tract (iris, ciliary body, and choroid). It can be anterior, intermediate, posterior, or pan‑uveitis, each affecting different eye layers.
- Conjunctivitis: Often called “pink eye,” this affects the thin membrane covering the white of the eye and the inside of the eyelids.
- Keratitis: Inflammation of the cornea, the clear front window of the eye, frequently linked to contact‑lens wear or microbial infection.

How Inflammation Impacts Vision
When the eye’s immune response goes awry, several mechanisms threaten visual clarity:
- Swelling of the iris or ciliary body can block the normal flow of aqueous humor, raising intraocular pressure. Persistent pressure spikes damage the optic nerve, leading to glaucoma‑related vision loss.
- Inflammatory cells and fluid can settle on the retina, causing retinal damage. Even minor macular edema can blur central vision permanently.
- Chronic inflammation often accelerates cataract formation, clouding the natural lens and reducing sharpness.
- Scar tissue on the cornea (from keratitis) creates irregular surfaces, scattering light and causing glare or ghost images.
Risk Factors and Underlying Conditions
Several systemic and local factors predispose a person to ocular inflammation:
- Autoimmune diseases such as rheumatoid arthritis, sarcoidosis, and ankylosing spondylitis can trigger uveitis.
- Diabetes mellitus increases susceptibility to infectious keratitis and can worsen inflammatory responses.
- Frequent contact‑lens wear, especially without proper hygiene, raises the risk of bacterial or fungal keratitis.
- Exposure to allergens, chemical irritants, or viral infections (e.g., herpes simplex) can ignite conjunctivitis.
Diagnosing and Monitoring Inflammation
Eye care professionals use a combination of clinical examination and imaging to assess severity:
- Slit‑lamp biomicroscopy lets the clinician view the front structures in high magnification, detecting cells, flare, and corneal lesions.
- Fundus photography and optical coherence tomography (OCT) reveal retinal swelling or vitreous infiltrates.
- Measurement of intraocular pressure with a tonometer tracks glaucoma risk.
- Blood tests (e.g., HLA‑B27 typing) and infectious panels help pinpoint systemic triggers.
Regular follow‑up is crucial; some forms of uveitis can flare weeks after an initial “quiet” period.

Treatment Options: From Topical Drops to Systemic Therapy
The therapeutic goal is to quiet the inflammation, protect ocular structures, and restore visual function. The choice of medication depends on location, severity, and underlying cause.
| Condition | Typical Cause | Main Symptoms | Risk to Vision | First‑Line Treatment |
|---|---|---|---|---|
| Uveitis | Autoimmune, infections, trauma | Redness, pain, photophobia, blurred vision | High - can cause glaucoma, cataract, retinal scarring | Corticosteroids (topical or systemic) + pupil‑dilating drops |
| Conjunctivitis | Viral, bacterial, allergic agents | Watery discharge, itching, mild redness | Low - rarely threatens vision unless severe bacterial | Antibiotic ointment (bacterial) or antihistamine drops (allergic) |
| Keratitis | Contact‑lens misuse, microorganisms, trauma | Severe pain, corneal opacity, light sensitivity | Medium to high - can lead to scarring and permanent vision loss | Broad‑spectrum antibiotics or antifungals; sometimes Immunosuppressants for immune‑mediated cases |
When corticosteroids aren’t enough or cause side effects, clinicians may add immunosuppressants such as methotrexate, azathioprine, or biologic agents (e.g., adalimumab). In infectious cases, targeted antibiotics or antivirals are essential. Occasionally, surgical interventions-like vitrectomy for persistent vitreous inflammation-are required.
Prevention and Lifestyle Tips
While some inflammatory episodes are unavoidable, patients can lower their odds by adopting a few habits:
- Maintain strict contact‑lens hygiene: replace, clean, and store lenses as recommended.
- Protect eyes from UV light with sunglasses that block 99‑100% UVA/UVB.
- Manage systemic health-keep blood sugar stable, treat autoimmune flare‑ups promptly.
- Stay up‑to‑date on vaccinations (e.g., herpes zoster) that can reduce viral eye infections.
- Schedule regular eye exams, especially if you have a known risk factor.
Quick Checklist for Anyone Experiencing Eye Inflammation
- Note any redness, pain, discharge, or changes in vision.
- Stop using contact lenses immediately and discard the solution.
- Apply any prescribed drops exactly as directed-don’t skip doses.
- Seek urgent care if vision becomes blurry, light‑sensitive, or if you see halos around lights.
- Keep a record of systemic symptoms (joint pain, skin rashes) to discuss with your doctor.
Frequently Asked Questions
Can mild eye inflammation resolve without medication?
Yes, many cases of viral conjunctivitis or allergic irritation improve on their own within a week. Artificial tears, cool compresses, and avoiding irritants often speed recovery. However, any persistent redness or vision change warrants professional evaluation.
What signs indicate that inflammation is threatening vision?
Sudden blurry or double vision, halos around lights, loss of peripheral sight, or severe pain are red‑flag symptoms. They can signal glaucoma, macular edema, or corneal ulceration-conditions that need immediate treatment.
Are corticosteroid eye drops safe for long‑term use?
Short‑term corticosteroid drops are effective and generally safe. Prolonged use, however, can raise intraocular pressure and promote cataract formation. Doctors usually monitor pressure and taper the drops to minimize risk.
How do autoimmune diseases cause eye inflammation?
Autoimmune disorders generate systemic inflammatory mediators that can target eye tissues, especially the uveal tract. The immune system mistakenly attacks the eye’s own cells, leading to chronic uveitis that often recurs without systemic disease control.
Is there a link between diabetes and eye inflammation?
People with diabetes are more prone to infectious keratitis and can experience exaggerated inflammatory responses to minor injuries. High blood sugar also impairs corneal healing, making infections harder to clear.

Comments (10)
Benjamin Hamel October 13 2025
While the article claims to cover eye inflammation comprehensively, it somehow glosses over the profound systemic connections that actually drive many of these ocular pathologies. One could argue that without a deep dive into the immunological cascades, the piece feels superficial at best. Moreover, the emphasis on a quick assessment tool seems to trivialize a condition that, in severe cases, can precipitate irreversible photoreceptor loss. The author mentions corticosteroids but neglects to explore the nuances of intraocular pressure monitoring during long‑term therapy. It is also puzzling that the role of biologics, such as anti‑TNF agents, receives merely a passing mention despite their growing relevance. Equally concerning is the omission of patient‑specific risk stratification based on HLA‑B27 status, which could have provided actionable insight. The section on contact‑lens hygiene, although useful, repeats advice that most ophthalmologists already consider basic. In addition, the discussion of retinal edema fails to differentiate between cystoid macular edema and serous detachment, both of which have distinct management pathways. The article could have benefited from a more robust exploration of optical coherence tomography findings, especially regarding vitreous haze quantification. Finally, the brief mention of UV protection does not address the emerging data on blue‑light filter lenses and their potential to mitigate inflammation‑induced oxidative stress. All these gaps suggest that the piece, while well‑intentioned, might leave a knowledgeable reader wanting more depth and precision.
Christian James Wood October 14 2025
Honestly, the whole tone of the write‑up feels like a corporate health brochure trying to sound caring while actually hiding the scary truth about how quickly inflammation can cripple your vision. If you think a simple checklist will save you from a potential glaucoma attack caused by unchecked uveitis, you’re being naive. The author barely scratches the surface of systemic autoimmune triggers, which are the real culprits behind chronic eye inflammation. It’s almost as if they’re deliberately downplaying the urgency to keep readers from freaking out, but that’s a disservice. You need to know that untreated macular edema can lead to permanent central vision loss within weeks, not months. Also, the suggestion to “monitor symptoms closely” is laughable when you consider how many patients ignore subtle photophobia until it’s too late. The piece should have shouted louder about the necessity of immediate specialist referral once intraocular pressure spikes. In short, readers deserve a stark warning, not a vague reassurance.
Rebecca Ebstein October 15 2025
Wow, this article really opened my eyes! Im super grateful for the checklist, it makes me feel more control over my eye health. Dont forget to keep ur contact lenses clean, that small step can save you big pain later. Stay positive and remember that many inflamation issues get better with proper care :)
Artie Alex October 16 2025
The preceding commentary fails to address the mechanistic underpinnings of cytokine‑mediated blood‑ocular barrier disruption, which is pivotal in the pathogenesis of uveitic sequelae. A more rigorous exposition would incorporate quantifiable biomarkers such as aqueous IL‑6 concentrations and their correlation with clinical grading scales. Moreover, the omission of differential diagnosis algorithms for masquerade syndromes reflects a lapse in scholarly thoroughness. Integrating vitreoretinal imaging parameters, specifically optical coherence tomography‑angiography metrics, would enhance diagnostic fidelity. Finally, the recommendation hierarchy should be restructured to prioritize steroid-sparing agents in patients with pre‑existing ocular hypertension.
abigail loterina October 17 2025
Great points! I think it’s important to keep the language simple so everyone can understand. Let’s remember to follow up with eye docs regularly.
Roger Cole October 18 2025
Thanks for the practical tips.
Krishna Garimella October 19 2025
It's amazing how a small habit like consistent lens hygiene can be a game‑changer for long‑term ocular health. Think of it as a meditation for your eyes-each cleaning step reinforces protection against hidden bacterial foes. Yet, beyond hygiene, embracing a balanced diet rich in omega‑3s fuels anti‑inflammatory pathways that support retinal resilience. While technology offers eye‑tracking apps for symptom logging, remember that mindful rest and screen breaks are equally vital. Together, these practices form a holistic shield against the insidious creep of inflammation.
nalina Rajkumar October 19 2025
Loving the vibes here 😃 Keep those eyes safe and happy 🙌
Daisy Aguirre October 20 2025
Reading this feels like a friendly reminder from a wise elder about caring for one of our most precious senses. The cultural nuance of protecting eyes from harsh sunlight parallels many traditions that value respect for the body. It's uplifting to see actionable steps woven with scientific insight, especially the emphasis on regular check‑ups for those with autoimmune backgrounds. Your mention of UV‑blocking sunglasses reminds me of the vibrant shades we wear during festivals, blending safety with style. And the suggestion to stay hydrated? Simple yet powerful for tear film stability. Overall, this piece balances education with encouragement, making the daunting topic of eye inflammation feel approachable.
Natalie Kelly October 21 2025
Super helpful, thanks! Will definitely schedule my next eye exam.