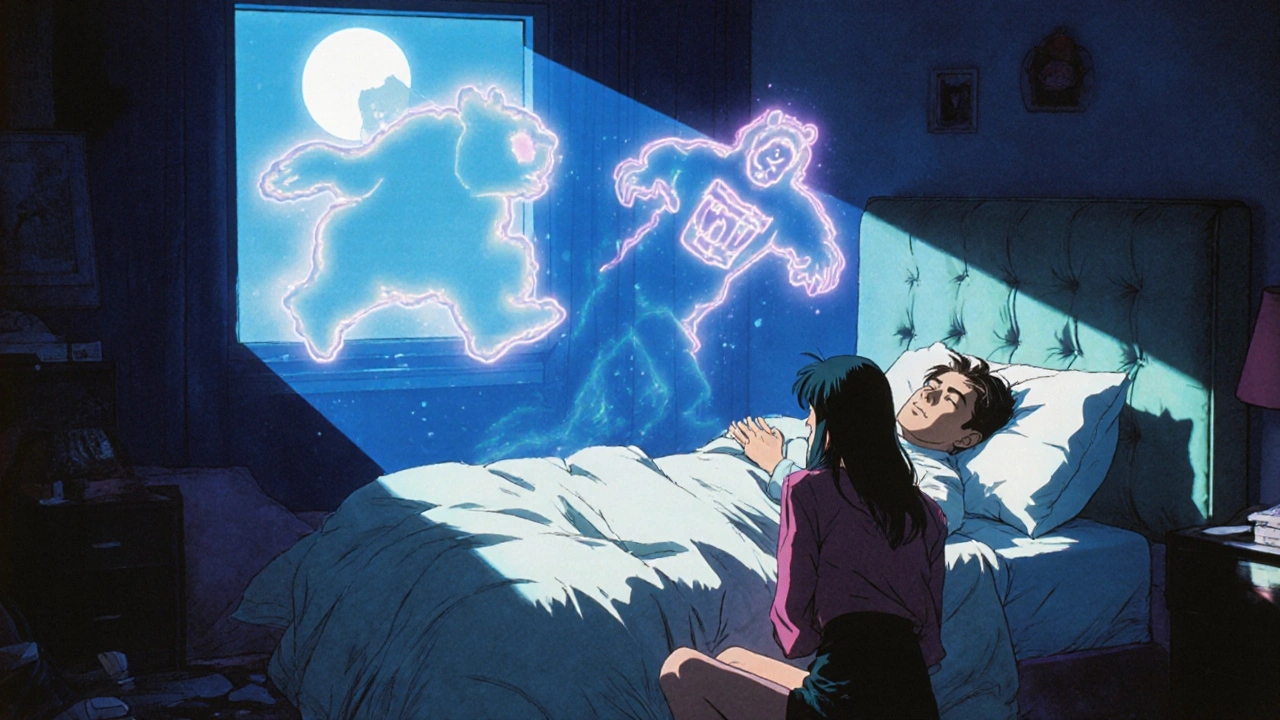
REM sleep behavior disorder isn't just about acting out dreams. It’s a warning sign your brain is changing in ways that could lead to Parkinson’s, dementia with Lewy bodies, or other serious neurological conditions. People with RBD punch, kick, yell, or even jump out of bed while asleep-often without remembering it the next morning. These aren’t bad dreams. They’re physical reactions caused by a breakdown in the brain’s normal ability to paralyze muscles during REM sleep. Left untreated, this disorder can lead to serious injuries, broken relationships, and sleepless nights for both the patient and their partner. But there’s more: RBD often appears years, sometimes decades, before the first signs of neurodegeneration. That makes it one of the clearest early indicators we have for future brain disease.
What Happens in the Brain During RBD?
Normally, when you enter REM sleep, your brain sends signals to temporarily shut down your major muscles. This prevents you from acting out your dreams. In RBD, that signal fails. The brainstem circuits responsible for muscle paralysis stop working properly. Instead of lying still, your body becomes active-mirroring what’s happening in your dreams. You might be dreaming about running from a bear, and suddenly you’re thrashing around the bed. Or you’re dreaming about arguing with someone, and you’re yelling or flailing your arms.
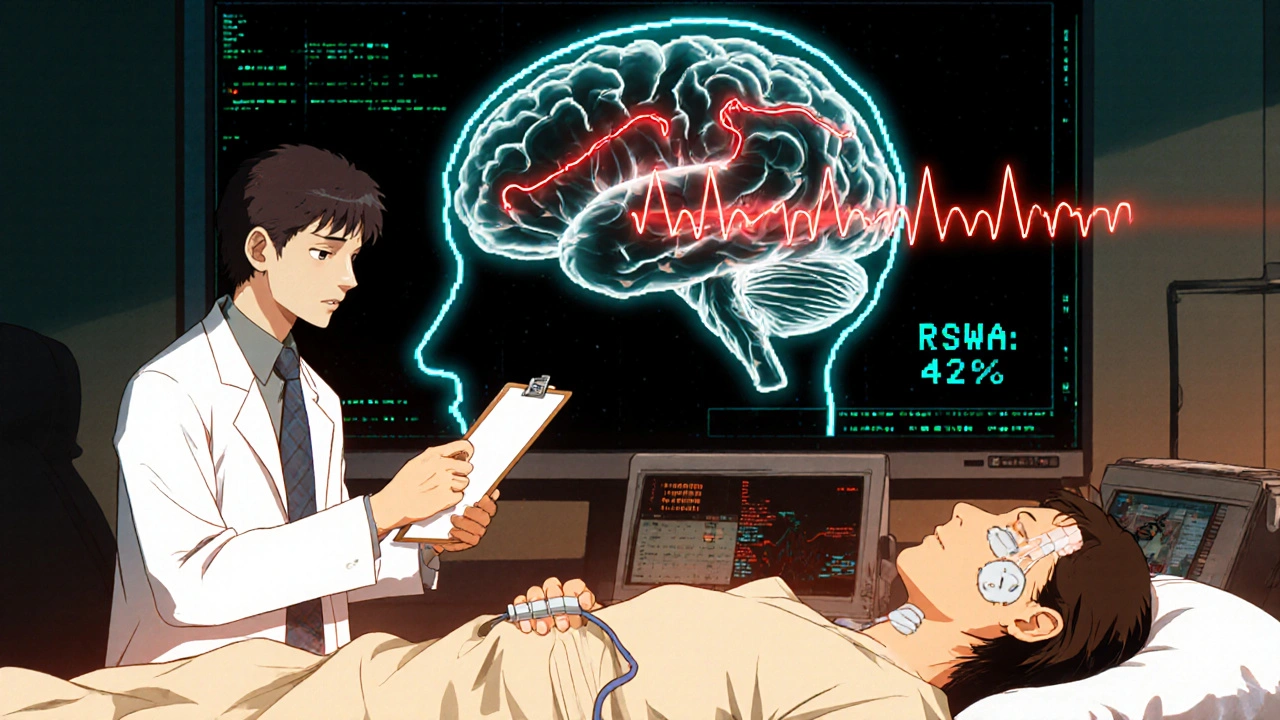
This isn’t just unusual behavior-it’s a measurable neurological event. The gold standard for diagnosis is a sleep study called polysomnography (PSG). During the test, electrodes track brain waves, eye movements, and muscle activity. The key finding? REM sleep without atonia (RSWA). That means your muscles are active during REM sleep when they should be completely still. According to the International Classification of Sleep Disorders, RSWA must be present in at least 15% of REM sleep epochs to confirm RBD. Studies show people with RBD average about 4.2 dream enactment episodes per hour, which adds up to dozens of dangerous movements over the course of a night.
Why Neurological Assessment Is Non-Negotiable
Getting diagnosed with RBD isn’t the end of the story-it’s the beginning of a long-term neurological watch. About 90% of RBD cases are linked to underlying synucleinopathies: Parkinson’s disease, dementia with Lewy bodies, or multiple system atrophy. A 2010 study found that 73.5% of people with idiopathic RBD (meaning no known cause) developed one of these conditions within 12 years. That’s not a small risk. It’s a near-certainty for many.
Because of this, the American Academy of Neurology recommends annual neurological exams for anyone diagnosed with RBD. These aren’t just checkups. They look for subtle signs of movement disorders: slight tremors, reduced arm swing while walking, changes in voice tone, or loss of smell-all early markers of Parkinson’s. A neurologist may also order brain imaging or autonomic function tests to detect changes before symptoms become obvious. The goal isn’t to predict the future, but to catch it early enough to intervene.
First-Line Treatments: Melatonin vs. Clonazepam
There are no FDA-approved drugs specifically for RBD. That means doctors rely on off-label options that have proven effective through decades of clinical use. The two most common are melatonin and clonazepam, both with different risk-benefit profiles.
Melatonin is a hormone your body naturally makes to regulate sleep. In RBD, supplemental melatonin helps restore the brain’s ability to suppress muscle activity during REM sleep. The typical starting dose is 3 mg taken at bedtime. Most patients gradually increase to 6 mg, 9 mg, or even 12 mg over several weeks. About 65% of people see significant improvement with melatonin alone. Side effects are mild: occasional morning grogginess, headaches, or dizziness. One 68-year-old patient reduced his weekly RBD episodes from seven to one after starting 6 mg nightly-only experiencing brief grogginess that faded after two weeks.
Clonazepam, a benzodiazepine, works by enhancing the effect of GABA, a calming neurotransmitter in the brain. It’s more potent than melatonin, with 80-90% of patients reporting symptom reduction. The usual starting dose is 0.25 mg to 0.5 mg at bedtime, with a maximum of 2 mg per night. Many see results within the first week. But it comes with serious trade-offs. Side effects include dizziness (22% of users), unsteadiness (18%), daytime sleepiness (15%), and memory issues. For older adults, the risk of falls increases by 34%. One patient stopped clonazepam after three months because his balance worsened-falls went from zero to two per month. Long-term use can also lead to dependence, and stopping abruptly causes rebound nightmares in 38% of cases.
Other Options and Emerging Therapies
Not everyone responds to melatonin or clonazepam. For those who don’t, doctors may try other medications. Pramipexole, a dopamine agonist used for Parkinson’s and restless legs syndrome, helps about 60% of RBD patients-especially those with overlapping leg movements. But it can cause nausea, swelling, and impulse control issues.
Rivastigmine, a cholinesterase inhibitor used in Alzheimer’s and dementia, showed promise in a small trial for RBD patients with mild cognitive impairment. It reduced dream enactment episodes when other treatments failed. But it’s not a first-line option due to limited evidence.
Looking ahead, the most exciting development is in dual orexin receptor antagonists. Orexin is a brain chemical that helps regulate wakefulness. Blocking both orexin receptors (OX1 and OX2) appears to stabilize sleep architecture and reduce muscle activity during REM. Mount Sinai researchers found a 78% reduction in dream enactment behaviors in animal models. Suvorexant (Belsomra), already approved for insomnia, is being studied for RBD. Neurocrine Biosciences’ drug NBI-1117568 received Fast Track designation from the FDA in January 2023 and is now in Phase II trials, with results expected in mid-2024. These drugs could offer the same effectiveness as clonazepam-with far fewer side effects.
Safety Comes First: Modifying the Sleep Environment
No medication works perfectly. Even with treatment, 42% of RBD patients eventually sleep separately from their partners due to safety concerns. That’s why environmental changes are just as important as drugs.
The Cleveland Clinic recommends these steps for every RBD patient:
- Remove all weapons from the bedroom-guns, knives, or tools.
- Pad sharp corners of furniture with foam or cushions.
- Place thick rugs or mats beside the bed to cushion falls.
- Install bed rails if mobility is impaired.
- Consider sleeping in a lower bed or on the floor temporarily.
Alcohol is a major trigger. Even one or two drinks can double the frequency of RBD episodes. Many patients report dramatic improvement after quitting alcohol entirely. Sleeping pills, sedatives, and certain antidepressants can also worsen symptoms. Always review your medications with a sleep specialist.
What to Expect During Treatment
Melatonin takes time. Don’t expect results after one night. Most patients need 2-4 weeks at each dose level (3 mg → 6 mg → 9 mg → 12 mg) before seeing full effects. Keep a sleep diary to track episodes, injuries, and side effects. Bring it to follow-up visits.
Clonazepam works faster-often within days-but tapering off requires patience. Reduce the dose by 0.125 mg every 1-2 weeks. Stopping too fast can cause nightmares, anxiety, or insomnia. Never quit cold turkey.
Track your neurological health. Annual checkups should include a full movement disorder exam. If you notice new stiffness, slower movements, or trouble with balance, tell your doctor right away. Early detection of Parkinson’s means earlier access to therapies that can slow progression.
The Bigger Picture: RBD as a Window to the Future
RBD is more than a sleep problem. It’s a neurological red flag. The same brain cells that fail in RBD are the ones that die in Parkinson’s and dementia with Lewy bodies. That’s why researchers are now treating RBD as a preclinical stage of neurodegeneration. The goal isn’t just to stop the kicks and yells-it’s to stop the brain from degenerating.
Drug companies are pouring money into this space. The global RBD market is worth $1.2 billion in 2023 and is projected to grow at 5.7% annually through 2030. The FDA now encourages development of RBD treatments as a way to delay or prevent neurodegenerative disease. Clinical trials are underway to test whether drugs that protect neurons can stop RBD from turning into Parkinson’s.
For now, the best approach is simple: treat the symptoms, protect the person, and monitor the brain. With the right combination of medication, safety changes, and regular checkups, most people with RBD can sleep safely-and live longer, healthier lives.

Comments (12)
Jenny Lee November 17 2025
My dad had RBD and started on 3mg melatonin-within two weeks, he stopped kicking the dog out of bed. No more broken lamps. Just quiet nights. I wish more people knew this wasn’t just ‘weird dreaming.’
Scott Macfadyen November 18 2025
Clonazepam saved my marriage. But now I’m scared to quit. I’ve been on it for 5 years and the nightmares come back like a freight train if I skip a dose. Not worth it for the dizziness, but damn if I know what else to do.
Denise Cauchon November 18 2025
MY GOD. I KNEW SOMETHING WAS WRONG WHEN MY HUSBAND STARTED YELLING AT THE WALLS IN HIS SLEEP. 😭 WE’RE SLEEPING IN SEPARATE ROOMS NOW. HE’S ON 12MG OF MELATONIN AND STILL KICKS THE BEDFRAME. THIS ISN’T A ‘SLEEP PROBLEM’-IT’S A NIGHTMARE THAT NEVER ENDS.
Andrea Johnston November 18 2025
Of course the medical establishment treats this like a nuisance. They’ll give you melatonin and call it a day while your brain slowly turns to mush. This isn’t sleep hygiene-it’s neurodegeneration on a timer. And no one’s talking about the real cost: the loneliness of sleeping alone because your partner’s afraid you’ll break their collarbone.
Jeff Hakojarvi November 20 2025
Just wanted to say-don’t panic if you’re diagnosed. I had RBD diagnosed 8 years ago. Had my first tremor last year. Started physical therapy, got a sleep study every 6 months, switched to melatonin + bed rails. Still live alone, still sleep well. It’s not a death sentence. It’s a heads-up. Use it.
Evan Brady November 21 2025
That dual orexin antagonist stuff? Pure gold. Imagine a pill that tamps down the dream chaos without turning you into a zombie. Suvorexant’s already FDA-approved for insomnia-why isn’t it being pushed for RBD like a damn priority? Pharma’s dragging their feet while people fall out of beds and break hips.
mithun mohanta November 23 2025
...and yet, the ‘neurological watch’ is just a capitalist trap. You pay for annual exams, you pay for melatonin, you pay for bed rails... while Big Pharma quietly patents the next ‘miracle drug’ that’ll cost $12,000/year. RBD is a goldmine. The real disease? Profit-driven healthcare.
Chloe Sevigny November 25 2025
It’s fascinating how RBD operationalizes the Cartesian dualism of mind and body-except here, the mind doesn’t merely inhabit the body, it violently disowns it during REM. The brainstem’s failure to inhibit motoneurons is not merely a physiological anomaly; it’s a metaphysical rupture. We are, in essence, dreaming in the raw, unfiltered substrate of motor output. And yet, we call it a ‘sleep disorder.’ How quaint.
Timothy Uchechukwu November 27 2025
Why do westerners always think they’re the first to notice brain problems? In my village in Nigeria, we’ve always known that people who act out dreams are cursed or possessed. We don’t need polysomnography. We just pray. And it works better than your pills. You think your science is better? You’re just scared of what you don’t understand
Ancel Fortuin November 28 2025
Let me guess-the real reason they’re pushing melatonin is because it’s cheap and unpatentable. Meanwhile, the same people who tell you to ‘monitor your brain’ are also the ones who refused to fund a cure for 30 years. Wake up. This isn’t medicine. It’s a controlled experiment. They want you to get Parkinson’s so they can sell you the next $800/month drug.
Ram tech November 29 2025
who even has time for all this? i got a 9-5 and my wife says i snore. i dont even know if im acting out dreams. maybe i just need to sleep less. or drink less coffee. or stop watching horror movies before bed. this whole thing feels like overdiagnosis
Victoria Malloy November 30 2025
Thank you for writing this. My mom was diagnosed last year. She’s on 9mg melatonin now, sleeps in a padded room, and we check on her every night. It’s scary-but reading this made me feel less alone. You’re not just treating a symptom. You’re protecting someone you love.