When you’re pregnant and have asthma, every decision about your health feels heavier. You’re not just thinking about yourself anymore-you’re thinking about your baby. Is that inhaler safe? Will my meds cause birth defects? Should I stop taking them just in case? These aren’t just fears-they’re real concerns millions of women face every year. The truth is, uncontrolled asthma is far more dangerous to your baby than the medications used to treat it.
Why Asthma Control Matters More Than You Think
Asthma affects between 4% and 12% of pregnant women worldwide. For many, symptoms stay the same during pregnancy. For others, they get worse-especially between weeks 24 and 36. That’s not random. Your body changes. Hormones shift. Your lungs have less room. If your asthma isn’t managed, your baby doesn’t get enough oxygen. That can lead to preterm birth, low birth weight, or even preeclampsia. Studies show that women with uncontrolled asthma are 1.3 times more likely to deliver early and 1.2 times more likely to have a baby with low birth weight.
It’s not about being “scared” of meds. It’s about understanding risk. The biggest danger isn’t the inhaler-it’s the asthma attack. A single severe flare-up can reduce oxygen flow to your baby for hours. And repeated flares? That’s a pattern that harms development. The goal isn’t to be symptom-free. It’s to keep your lungs working well enough to support two lives.
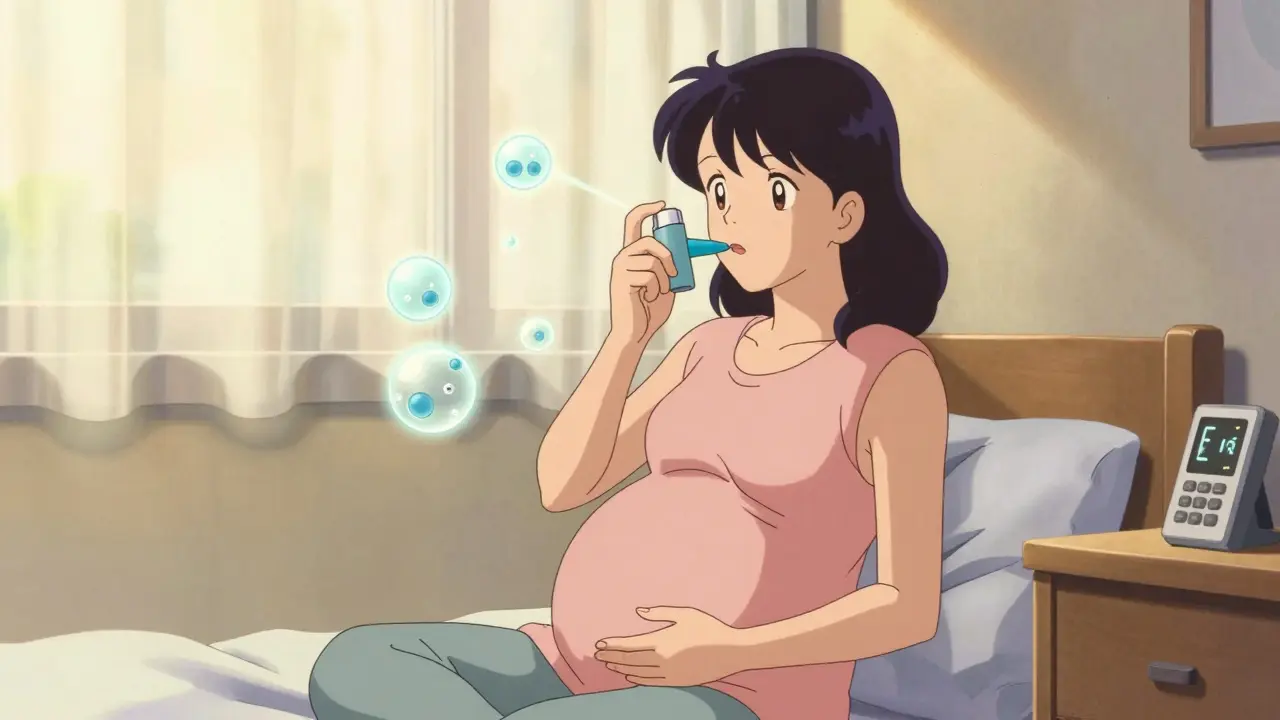
What Asthma Medications Are Safe During Pregnancy?
Not all asthma drugs are created equal-especially when you’re pregnant. But here’s the good news: most inhaled asthma medications are safe. They work right where they’re needed: in your lungs. Very little enters your bloodstream. Even less reaches your baby.
Inhaled corticosteroids (ICS) are the first-line treatment. Among them, budesonide has the strongest safety record. Over 1,000 documented pregnancies show no increased risk of birth defects. It’s the most studied, most trusted option. Beclomethasone and fluticasone propionate are also considered safe, with decades of data backing them up.
For quick relief during an attack, albuterol (salbutamol) and levalbuterol are safe. A review of 1.2 million pregnancies found no link to birth defects. These are your rescue inhalers-use them without guilt when you need them.
If you need daily control beyond ICS, formoterol and salmeterol (long-acting beta-agonists) are safe when used with an ICS. They’re not for rescue-they’re for prevention. And if you’re on montelukast (Singulair), don’t panic. Over 1,000 pregnancies studied show no increase in major malformations.
Medications to Avoid or Use With Caution
Some asthma treatments carry more risk during pregnancy-and that’s why doctors avoid them unless absolutely necessary.
Oral corticosteroids like prednisone or methylprednisolone are the biggest red flag. A 2023 study of 1.8 million pregnancies found a 30-60% higher risk of cleft lip or palate when taken in the first trimester. They also raise the chance of preterm birth and low birth weight. If you need them for a severe flare, your doctor will use the lowest dose for the shortest time possible. But they’re not for daily use.
Theophylline is rarely used today. It works, but it needs blood tests to make sure levels are safe. Too much can cause nausea, rapid heartbeat, or even seizures. It’s not dangerous-but it’s harder to manage than inhaled meds.
Tiotropium (Spiriva) has almost no safety data in pregnancy. Only 324 pregnancies have been tracked. Until more evidence exists, experts recommend avoiding it as a first choice.
Newer biologics like omalizumab, mepolizumab, or dupilumab? Omalizumab has data from over 700 pregnancies with no increased risk. But the rest? Too few women have been studied. They’re not banned-but they’re not recommended unless you have life-threatening asthma and no other options.
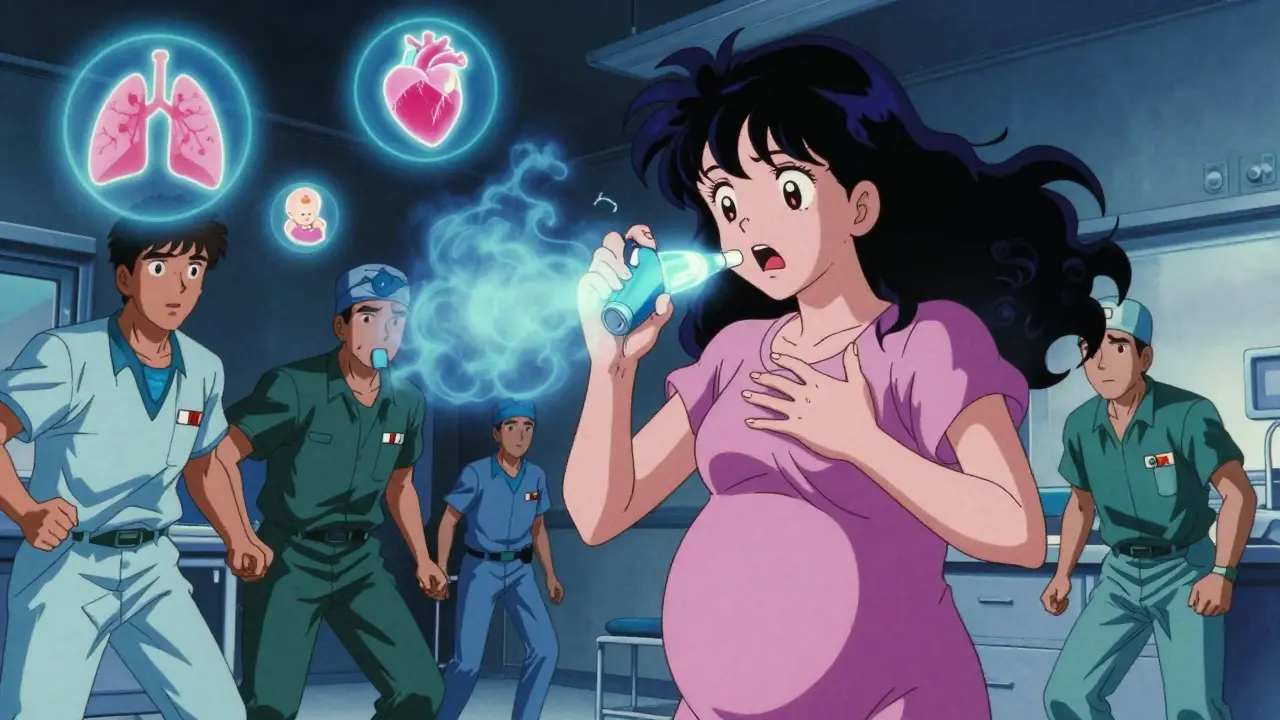
What Happens If You Stop Your Medication?
Many women stop their asthma meds out of fear. It’s understandable. But here’s what happens next:
- 41% of women who stopped inhaled steroids during pregnancy had at least one severe asthma attack needing emergency care.
- Only 17% of women who kept taking their meds had the same outcome.
- Women who discontinued treatment were 2.5 times more likely to be hospitalized for asthma during pregnancy.
It’s not just about breathing. Uncontrolled asthma increases the risk of gestational diabetes, high blood pressure, and even stillbirth. Your baby’s lungs need steady oxygen to grow. Your body needs steady control to stay healthy.
One mother on a support forum said: “I stopped my inhaler because my OB said ‘maybe it’s better not to.’ I had three ER visits by week 30. I felt like I was failing my baby. I started back on budesonide and didn’t have another flare.”
How to Monitor Your Asthma During Pregnancy
Managing asthma isn’t just about pills and inhalers. It’s about tracking. You need to know if your control is slipping before it becomes an emergency.
- Use a peak flow meter daily. Your goal: stay above 80% of your personal best. If it drops below 70%, call your doctor.
- Keep an asthma symptom diary. Note wheezing, coughing, nighttime symptoms, and how often you use your rescue inhaler.
- Take the Asthma Control Test (ACT) every 4 weeks. A score of 20 or higher means your asthma is under control. Below 20? You need a plan change.
- Track your oxygen levels with a pulse oximeter if recommended. Keep them above 95%.
Monthly check-ins with your asthma specialist are critical. And if you’re seeing an OB, make sure they’re talking to your pulmonologist or allergist. Joint visits at 8, 16, 24, and 32 weeks are the gold standard for moderate to severe asthma.
Environmental Triggers to Reduce
Medication isn’t the only tool. Avoiding triggers can cut your flare-ups in half.
- Use allergen-proof mattress and pillow covers. They reduce dust mite exposure by 83%.
- Keep indoor humidity between 30% and 50%. Higher than that? Mold grows. Lower? Dry air triggers coughing.
- Remove carpets. They trap allergens. Hard floors are easier to clean and safer for your lungs.
- Avoid smoke-cigarettes, fireplaces, candles. Even secondhand smoke increases asthma attacks by 40%.
- Wash bedding weekly in hot water (130°F or higher).
These aren’t “nice-to-haves.” They’re part of your treatment plan. And they work.
What About New Treatments and Research?
Science is catching up. The FDA stopped using old pregnancy categories (A, B, C, D, X) in 2015. Now, labels give clear explanations: “There is no evidence of risk in humans,” or “Risk cannot be ruled out.” That’s better-but still confusing.
Research is growing. A $15.2 million NIH study launched in 2024 is tracking 2,500 children born to asthmatic mothers to see if asthma meds affect brain development. Early data suggests no harm-but we need more.
And there’s hope on the horizon: genetic testing may soon tell us which women respond best to specific inhalers. For example, 28% of women carry a gene variant that makes them respond better to budesonide. That could mean personalized asthma care during pregnancy-right down to the right inhaler for your body.
What You Should Do Right Now
If you’re pregnant and have asthma:
- Don’t stop your meds without talking to your doctor.
- Make sure your asthma action plan is updated for pregnancy.
- Ask for a referral to an allergist or pulmonologist if you don’t have one.
- Start using a peak flow meter if you aren’t already.
- Track your symptoms and share them at every appointment.
- Ask about budesonide if you’re on another steroid-it’s the gold standard.
And if you’re scared? You’re not alone. But you’re not powerless. The right treatment lets you breathe. And when you breathe well, your baby breathes well too.
Is it safe to use an inhaler while pregnant?
Yes, most inhalers are safe during pregnancy. Inhaled corticosteroids like budesonide, beclomethasone, and fluticasone propionate have strong safety data and are recommended as first-line treatment. Rescue inhalers like albuterol are also safe and should be used as needed. These medications deliver the drug directly to the lungs, with minimal absorption into the bloodstream and even less reaching the baby.
Can asthma medications cause birth defects?
The risk from properly used asthma medications is extremely low. Over 1,000 pregnancies studied with budesonide show no increase in birth defects. For albuterol, data from 1.2 million pregnancies found no link to congenital malformations. The real danger comes from uncontrolled asthma, which increases the risk of complications like preterm birth and low birth weight far more than any asthma medication.
Should I stop my asthma meds if I’m planning to get pregnant?
No. Stopping asthma medication before or during pregnancy increases the risk of flare-ups, which can harm both you and your baby. The best approach is to work with your doctor to optimize your treatment plan before conception. Budesonide is often the preferred choice for women planning pregnancy due to its strong safety record.
Are oral steroids like prednisone safe during pregnancy?
Oral corticosteroids like prednisone carry higher risks and are not recommended for routine use during pregnancy. Studies show they increase the chance of cleft lip or palate by 30-60% when used in the first trimester, and raise risks of preterm birth and low birth weight. They should only be used short-term for severe asthma attacks, under close medical supervision.
How often should I see my doctor for asthma during pregnancy?
Women with moderate to severe asthma should have coordinated care between their OB and asthma specialist. Recommended check-ups are at 8, 16, 24, and 32 weeks. Monthly monitoring with peak flow measurements and asthma control tests helps catch problems early. If your asthma is well-controlled, your doctor may adjust visits-but don’t skip them.
Can I breastfeed while taking asthma medication?
Yes. Most asthma medications are safe during breastfeeding. Inhaled corticosteroids and bronchodilators like albuterol pass into breast milk in very small amounts, far below levels that would affect the baby. The benefits of breastfeeding and maintaining good asthma control far outweigh any theoretical risk. Continue your treatment as prescribed.

Comments (13)
Jason Jasper December 25 2025
I was terrified to use my inhaler when I got pregnant. Thought I’d be some kind of monster for taking meds. Turns out, skipping it almost got me hospitalized at 28 weeks. Budesonide saved me. My daughter’s two now-no issues, no delays, just a happy kid who loves loud music and peanut butter. You’re not harming your baby by treating asthma. You’re giving them a chance to breathe.
Carlos Narvaez December 27 2025
Actually, the data is cherry-picked. Most studies are funded by pharma. The real risk? Long-term epigenetic changes from inhaled steroids. We don’t have 20-year follow-ups. You’re trading one unknown for another.
Harbans Singh December 28 2025
As someone from India where asthma is often untreated due to cost, I’m glad this info is out there. My sister stopped her inhaler during pregnancy because she thought it was ‘too strong.’ She ended up in the ER twice. Now she uses budesonide and her son is thriving. Please don’t let fear silence you. Talk to your doctor. You’re not alone.
Justin James December 29 2025
Let me tell you what they don’t want you to know. The FDA didn’t just change labels-they erased the old categories because they were caught hiding data. The real danger isn’t asthma-it’s the corporate agenda pushing inhalers as ‘safe’ while the NIH quietly studies whether these drugs alter fetal neurodevelopment. That $15 million study? It’s not about safety-it’s damage control. They already know. They just need more time to bury it.
Zabihullah Saleh December 29 2025
It’s funny how we treat the body like a machine you can just plug meds into. But pregnancy isn’t a fix-it’s a transformation. Maybe the real question isn’t ‘is this drug safe?’ but ‘how do we honor the body’s need to adapt?’ I’ve seen women who stopped meds and found their asthma improved with yoga, breathing exercises, and less stress. Not everyone needs inhalers. Sometimes, the medicine is stillness.
Winni Victor December 31 2025
Oh wow, another ‘trust your doctor’ pep talk. How about we stop gaslighting pregnant women into taking chemicals they don’t understand? I’m not some lab rat for Big Pharma. My body knows what’s best. I’d rather risk a cough than risk my baby being born with a weird gene glitch.
Sophie Stallkind January 1 2026
It is imperative that expectant mothers consult with their obstetrician and pulmonologist prior to initiating or modifying any therapeutic regimen. The evidence base supporting the safety of inhaled corticosteroids, particularly budesonide, is robust and peer-reviewed. Discontinuation of therapy carries demonstrably higher morbidity for both maternal and fetal outcomes. Adherence to clinical guidelines is not merely advisable-it is medically obligatory.
sagar patel January 3 2026
Stop the fear. The data is clear. Budesonide is safe. Albuterol is safe. Stopping is not. Your baby needs oxygen more than it needs your fear.
Michael Dillon January 3 2026
My wife had asthma since she was 12. Got pregnant, kept her inhaler, used a peak flow meter religiously. Had a 9lb 3oz baby at 39 weeks. No NICU. No complications. She didn’t even need a C-section. The only thing that almost killed her? The lady at the OB’s office who told her to ‘wait and see’ if she got wheezy. Don’t be that lady.
Terry Free January 3 2026
Oh look, another ‘science says’ article written by someone who’s never had to choose between breathing and not poisoning their child. You call budesonide ‘safe’? What’s safe? When your kid turns 12 and gets ADHD because you pumped his developing brain with steroids while he was still a blob? Don’t act like this is just about oxygen. It’s about control. And you’re not the boss of my body.
Lindsay Hensel January 4 2026
This is one of the most compassionate, evidence-based guides I’ve ever read on maternal asthma. Thank you for not minimizing the fear-while also dismantling the myths. As a nurse who’s held the hands of too many women crying over their inhalers, I can say with certainty: knowledge is the antidote to panic.
Katherine Blumhardt January 6 2026
omg i just found this and i was about to stop my inhaler 😭 i had no idea budesonide was safe like i thought all steroids were bad like in movies?? i feel so dumb but also so relieved like i can finally sleep again??
Bailey Adkison January 7 2026
They say budesonide is safe but what about the 1 in 5000 cases where it causes a cleft palate? They bury that. You think you’re doing the right thing but you’re just trusting a system that’s been lying to you since the 70s. I’ve seen it. I’ve lost babies. Don’t be another statistic.