When you take an opioid for pain, it works - fast and strong. But what happens after a few weeks? Your body changes. The same dose doesn’t help as much. You need more. That’s not weakness. It’s biology. And it’s the first step toward something far more dangerous: dependence, tolerance, and the very real chance of dying from an overdose.
How Opioids Work - And Why They’re So Risky
Opioids like oxycodone, hydrocodone, morphine, and fentanyl bind to special receptors in your brain and spinal cord. These receptors control pain signals - but they also trigger dopamine release, which creates euphoria. That’s why they’re effective for pain, and why they’re so addictive.
But here’s the catch: the same receptors that block pain also control your breathing. Too much opioid, and your brain stops telling your lungs to breathe. That’s overdose. And it kills.
The risk isn’t just for people who misuse drugs. Even patients taking opioids exactly as prescribed can develop tolerance. Studies show that within six months of daily use, many people need 25-50% higher doses to get the same pain relief. That’s not failure - it’s how the brain adapts.
Tolerance Isn’t Just About Needing More
Tolerance means your body gets used to the drug. At the cellular level, opioid receptors become less responsive. They’re pulled inside the cell, their signaling slows down, and your body starts producing more chemicals that counteract the drug’s effects. This is called neuroadaptation.
But here’s the dangerous part: tolerance to pain relief and euphoria develops faster than tolerance to respiratory depression. That means you might need a higher dose to feel good or stop hurting - but your breathing still responds to the same deadly level of opioid in your blood.
That’s why someone who’s been taking high doses for months can still overdose. Their body is used to the high, but their breathing hasn’t caught up. This mismatch is why long-term users aren’t immune - they’re still at risk.
Dependence: When Your Body Can’t Function Without It
Tolerance leads to dependence. That’s when your body relies on the drug to feel normal. Stop taking it, and you get withdrawal: nausea, sweating, muscle aches, anxiety, insomnia. It’s not just uncomfortable - it’s physically terrifying.
Dependence doesn’t mean addiction. Addiction is when you keep using despite harm - lost jobs, broken relationships, health damage. But dependence is the biological foundation. You don’t choose it. It happens.
And here’s the cruel twist: once you’re dependent, stopping isn’t easy. Many people go back to opioids not because they want to get high, but because they can’t stand the withdrawal. That’s how the cycle traps people.

Overdose: The Silent Killer
In 2021, over 80,000 people in the U.S. died from opioid overdoses. Most of those deaths involved synthetic opioids - primarily fentanyl. Fentanyl is 50 to 100 times stronger than morphine. A few milligrams can kill. And it’s often mixed into other drugs without the user’s knowledge.
But overdose isn’t just about street drugs. Prescription opioids kill too. People who take high doses for chronic pain, especially when combined with alcohol, benzodiazepines, or sleep aids, are at serious risk. These drugs all slow breathing. Together, they can shut it down completely.
And here’s one of the most misunderstood facts: people who’ve been clean for weeks or months are at the highest risk of fatal overdose. Why? Because their tolerance drops. Their body forgets how to handle the drug. If they relapse and take their old dose - the one that used to feel fine - it can kill them.
One user on a recovery forum wrote: “After six months clean, I used my old dose. Paramedics said I was clinically dead for four minutes.” That’s not rare. Studies show 65% of opioid overdose deaths happen in people who’ve had prior treatment.
Why Some Opioids Are Safer Than Others
Not all opioids are the same. Buprenorphine, used in Medication-Assisted Treatment (MAT), is a partial agonist. It activates opioid receptors just enough to reduce cravings and withdrawal - but it has a ceiling. Even at high doses, it doesn’t suppress breathing the way full agonists like fentanyl or oxycodone do.
That’s why buprenorphine is one of the safest tools we have. It reduces overdose risk by about half. And since 2023, any licensed U.S. doctor can prescribe it - no special waiver needed. That’s a huge change.
Methadone also helps, but it’s trickier. It stays in your system longer, and the dose has to be carefully managed. Too much, and it can cause overdose - especially in people new to it.
Heroin is dangerous because its potency varies. One batch might be pure. The next might be cut with fentanyl. Users can’t tell the difference. That’s why overdose deaths spiked as fentanyl flooded the market.
The Real Shift: From Prescription to Illicit
In 2012, doctors wrote over 80 prescriptions for every 100 Americans. By 2021, that dropped to under 47. Tighter rules helped. But the problem didn’t go away - it got worse.
As prescriptions became harder to get, many people turned to heroin. Then came fentanyl. It’s cheap, potent, and easy to smuggle. Between 2015 and 2022, fentanyl seizures in the U.S. increased by 1,200%.
Today, synthetic opioids like fentanyl are involved in 70% of all opioid overdose deaths. That’s up from less than 20% in 2015. The epidemic has changed. The drugs are deadlier. And the risk isn’t just for people with a history of addiction - it’s for anyone who uses anything bought off the street.
What Actually Works to Prevent Overdose
There’s no magic fix. But some things save lives.
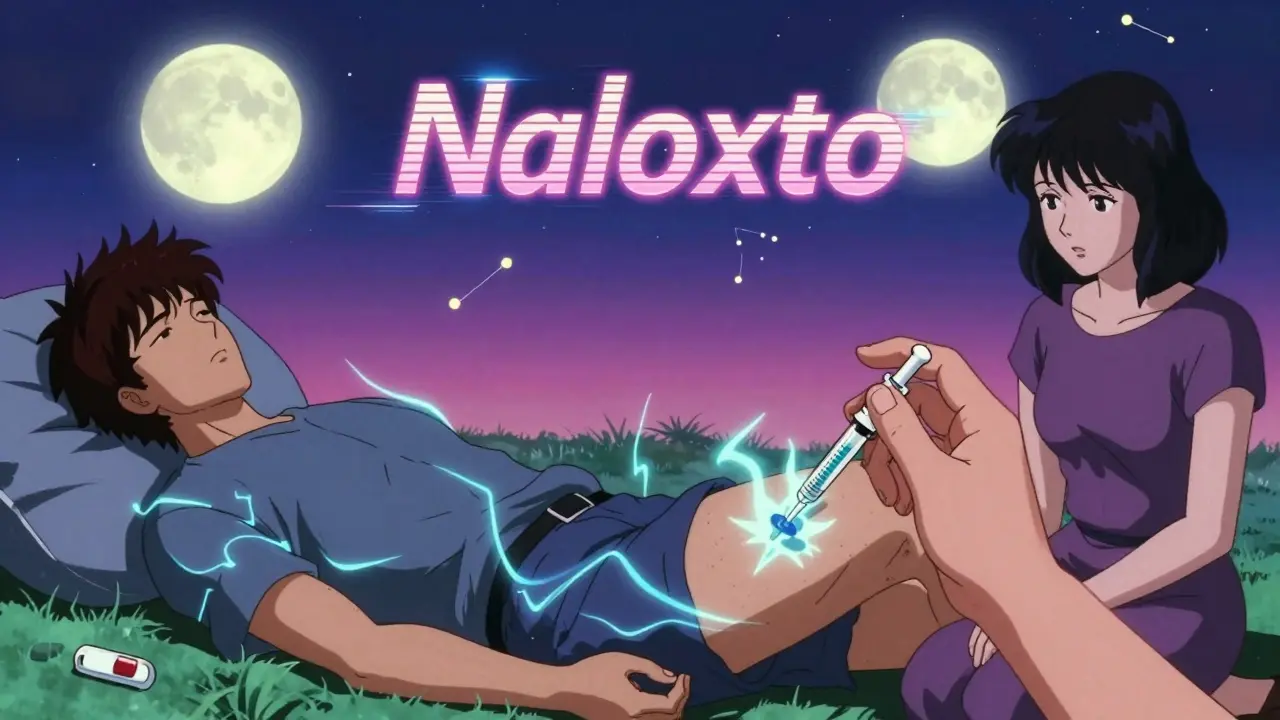
- Naloxone - It reverses overdose. It’s safe, easy to use, and works in minutes. Communities that hand it out for free have seen overdose deaths drop by 34%.
- Medication-Assisted Treatment (MAT) - Buprenorphine or methadone + counseling cuts overdose risk by half. It’s not replacing one drug with another. It’s giving people stability so they can rebuild their lives.
- Harm reduction - Clean needles, drug checking kits, supervised consumption sites. These don’t encourage use. They keep people alive until they’re ready to get help.
And here’s something most people don’t know: if you’re on long-term opioids for pain, talk to your doctor about naloxone. Even if you’ve never misused it, you’re still at risk. One study found that 32% of patients on chronic opioid therapy developed misuse behaviors within a year. You don’t have to be an addict to overdose.
What’s Next?
Researchers are working on new opioids that relieve pain without suppressing breathing. Early versions - called biased agonists - show promise in animal studies. They might one day separate the good effects from the deadly ones.
But right now, the best tools we have are simple: naloxone, buprenorphine, education, and compassion.
Opioids aren’t evil. They’re powerful tools that can help - if used carefully. But when tolerance builds, dependence forms, and overdose looms, the line between healing and harm becomes terrifyingly thin. Understanding that line isn’t just medical knowledge. It’s survival.
Can you develop tolerance to opioids even if you take them exactly as prescribed?
Yes. Tolerance is a biological response, not a sign of misuse. Even patients taking opioids exactly as directed for chronic pain often need higher doses over time. Studies show average dose increases of 25-50% within the first six months. This happens because opioid receptors become less responsive with prolonged use, requiring more of the drug to achieve the same effect.
Why are people who’ve been clean at higher risk of overdose when they relapse?
When someone stops using opioids, their body loses tolerance - especially to respiratory depression. Their brain and lungs no longer expect the drug. If they return to their previous dose, their body can’t handle it. This is why 65% of opioid overdose deaths occur in people with prior treatment history. A dose that once felt manageable can now be fatal.
Is fentanyl more dangerous than other opioids?
Yes. Fentanyl is 50 to 100 times more potent than morphine. A dose as small as 2 milligrams can be lethal. It’s often mixed into heroin, cocaine, or counterfeit pills without the user’s knowledge. In 2021, synthetic opioids like fentanyl were involved in 70.3% of all opioid overdose deaths in the U.S., up from just 19.5% in 2015.
Does buprenorphine help prevent overdose?
Yes. Buprenorphine is a partial opioid agonist with a ceiling effect on respiratory depression. That means it reduces cravings and withdrawal without causing dangerous breathing problems at typical doses. Studies show it cuts overdose risk by about 50%. Since 2023, any licensed U.S. doctor can prescribe it, making it far more accessible than before.
Can naloxone reverse any opioid overdose?
Naloxone reverses overdoses caused by opioids, including heroin, fentanyl, oxycodone, and morphine. It works by kicking the opioid off the brain’s receptors and restoring breathing. It doesn’t work on non-opioid drugs like cocaine or methamphetamine. But for opioid overdoses, it’s fast, safe, and life-saving - even if you’re not sure what was taken.
Are prescription opioids safer than street drugs?
Not necessarily. While prescription opioids are dosed more predictably, they still carry high risks of tolerance, dependence, and overdose - especially when combined with alcohol or other sedatives. And since 2021, most opioid overdose deaths involve illicit fentanyl, not prescription pills. But many people who start with prescriptions end up switching to street drugs when access is cut off. The danger is the same: opioids suppress breathing, no matter where they come from.


Comments (9)
michelle Brownsea January 20 2026
Let me be perfectly clear: tolerance isn't a biological accident-it's a predictable, avoidable consequence of prescribing opioids like candy. We've normalized this. We've let doctors hand out pills like they're giving out lollipops at a kindergarten party-and then act shocked when people die? No. No, no, no. This isn't 'biology'-it's negligence dressed up as compassion. And yes, I'm calling out every prescriber who didn't exhaust non-opioid options first. Your 'pain management' is a death sentence with a prescription pad.
Malvina Tomja January 21 2026
Let’s not romanticize this. Tolerance is not a neutral physiological process-it’s a surrender. The brain doesn’t ‘adapt’-it capitulates. And when you capitulate to opioids, you don’t just lose pain relief-you lose autonomy. The moment you need more to feel ‘normal,’ you’ve already lost. The fact that we call this ‘biological’ instead of ‘addictive’ is the real tragedy. Language is the first lie we tell ourselves to avoid responsibility.
Samuel Mendoza January 21 2026
Naloxone doesn't fix the problem. It just lets people keep using. We're not saving lives-we're prolonging the disaster.Steve Hesketh January 22 2026
Man, I’ve seen this up close-cousin took opioids after a back surgery, went from ‘just for a while’ to needing a whole pharmacy just to feel human. Not because he was weak, not because he wanted to get high-but because his body screamed at him every morning like it was on fire. Then he found buprenorphine. Didn’t fix everything-but gave him back his voice. His kids say he laughs again. That’s not magic. That’s medicine. And we need more of it, not less.
Sangeeta Isaac January 22 2026
so like… if i take my oxycodone like a good lil patient and then one day my doc says ‘sorry no more’ and i go to buy some fentanyl-laced ‘oxys’ off a guy named ‘dave’ who lives in a van… is that my fault? or is it the system’s fault for making me choose between agony and death? 🤔 also why is it always the poor folks who get the deadly cocktails and the rich folks get to go to rehab with yoga and kale smoothies? just sayin’.
Alex Carletti Gouvea January 23 2026
Why are we letting foreign fentanyl kill Americans? China’s behind this. This isn’t a health crisis-it’s an act of war. We need military lockdowns on the border, not pamphlets and naloxone. This isn’t ‘compassion’-it’s surrender.
Jerry Rodrigues January 24 2026
I’ve been on chronic pain meds for 12 years. I never got high. I never lied to doctors. I never bought anything off the street. But yeah-I needed higher doses. And yeah-I was terrified of withdrawal. I didn’t want to be dependent. But I didn’t want to scream through the night either. Naloxone saved me once. I carry it like a seatbelt. Doesn’t mean I’m a junkie. It means I’m smart.
Jarrod Flesch January 25 2026
Just wanna say-buprenorphine is a game changer. My mate was on 120mg oxycodone a day. After 3 months on suboxone? He’s working again. Sleeping through the night. Playing guitar. No euphoria. No crashing. Just… peace. And yeah, he still needs it. But now it’s keeping him alive, not killing him. 🙏
Also-naloxone kits should be in every pub, school, and gas station. Like fire extinguishers. No stigma. Just safety.
Barbara Mahone January 25 2026
There’s a quiet dignity in suffering without euphoria. Many of us take opioids not for pleasure, but to exist. To sit with our children. To hold our partner’s hand. To breathe without flinching. The stigma assumes we want to escape. But sometimes, we just want to be present. That’s not weakness. That’s endurance.