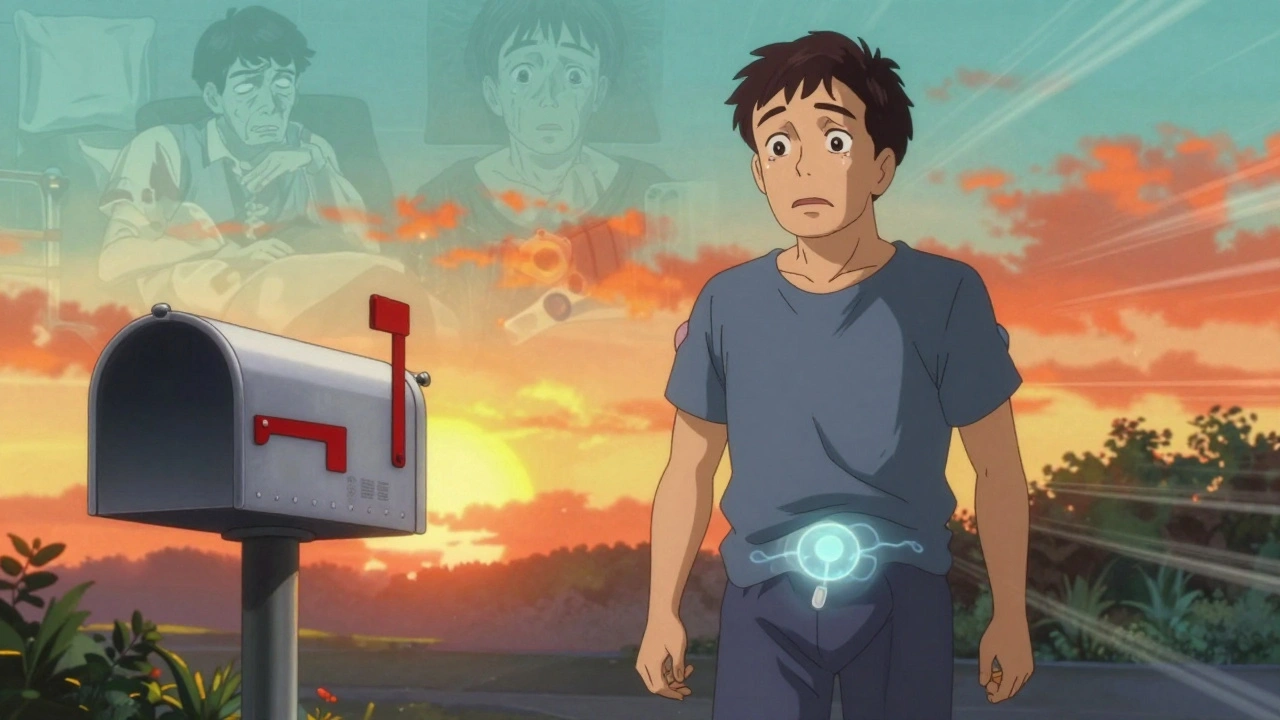
Chronic pain doesn’t just hurt-it steals your life. You can’t sleep. You can’t walk. You can’t work. And after years of pills, injections, and physical therapy, nothing seems to stick. That’s where spinal cord stimulation comes in. It’s not a cure. But for many, it’s the first real chance at getting back some control.
What Spinal Cord Stimulation Actually Does
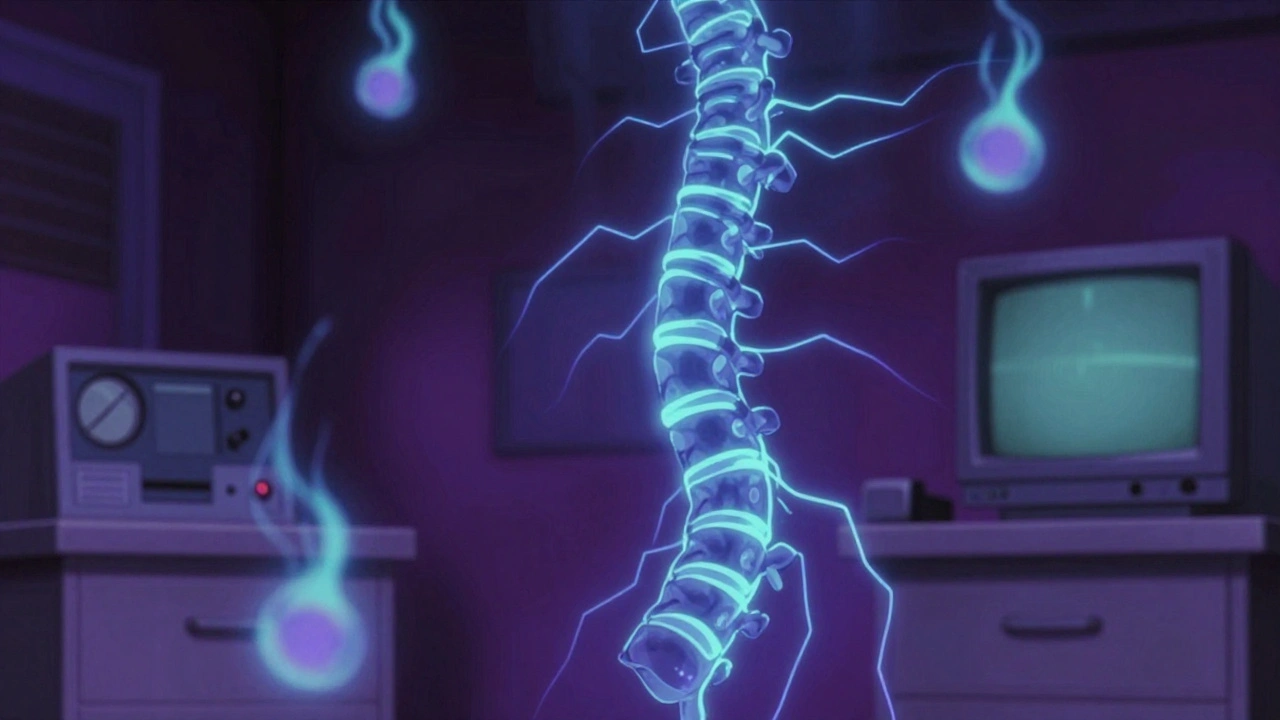
Spinal cord stimulation (SCS) uses mild electrical pulses to interrupt pain signals before they reach your brain. Think of it like static on a radio-instead of hearing the scream of pain, you hear a quiet hum, or sometimes, nothing at all. Electrodes are placed in the epidural space near your spine, connected to a small generator implanted under your skin, usually in your abdomen or buttock. The device doesn’t fix the source of the pain. It changes how your brain perceives it.
This isn’t new. The first system was tested in 1967. But today’s devices are light-years ahead. Older models relied on tingling sensations (paresthesia) to mask pain. Newer ones-like Boston Scientific’s WaveWriter Alpha™ Prime and Medtronic’s Intellis™-use high-frequency pulses (up to 10,000 Hz) or burst patterns that deliver relief without any tingling. In clinical trials, 89% of patients using these newer systems reported paresthesia-free pain relief.
Who Is a Good Candidate?
Not everyone with chronic pain is a candidate. SCS isn’t for backaches from lifting heavy boxes or arthritis flare-ups. It’s for persistent, nerve-based pain that hasn’t responded to anything else. The best candidates typically:
- Have tried physical therapy, medications, and injections for at least 6-12 months with no lasting results
- Have a clear diagnosis-like failed back surgery syndrome, complex regional pain syndrome (CRPS), or neuropathic leg pain
- Are not dependent on high-dose opioids (or are actively trying to reduce them)
- Have no untreated mental health conditions like major depression or anxiety
Psychological screening is just as important as imaging. A 2022 study found patients with untreated depression had 35% lower success rates. If you’re struggling with mood, SCS won’t fix that-therapy or medication should come first.
And you need to pass a trial. Before implant, you’ll wear an external device for 5-7 days with temporary leads. If your pain drops by 50% or more, you’re likely a good fit. If not, the permanent implant won’t help.
How It Compares to Other Options
Let’s be honest-no pain treatment is perfect. Here’s how SCS stacks up:
| Treatment | Effectiveness | Invasiveness | Cost (USD) | Long-Term Use |
|---|---|---|---|---|
| Spinal Cord Stimulation (SCS) | 50-85% achieve ≥50% pain reduction | Surgical (implant) | $25,000-$45,000 | 5+ years (with battery replacements) |
| Opioid Medications | Short-term relief only; high risk of dependence | Non-invasive | $500-$2,000/year | Not sustainable |
| TENS Unit | Under 30% for chronic pain | Non-invasive | $50-$200 | Temporary relief only |
| Peripheral Nerve Stimulation | Good for localized pain (e.g., knee), poor for back | Surgical (smaller implant) | $20,000-$35,000 | 3-5 years |
SCS cuts opioid use by over half after two years, according to a 2021 JAMA study. That’s huge. But it’s not magic. You still need to move, stretch, and manage stress. The device helps you do those things without being paralyzed by pain.
The Two-Step Process
Getting SCS isn’t a one-and-done deal. It’s a two-phase journey.
- Trial Phase: Temporary leads are threaded through your back using fluoroscopic guidance. You’re awake but sedated. The external generator is taped to your skin. You go home for a week, logging pain levels and adjusting settings. If it works, you move forward.
- Permanent Implant: A 60-90 minute surgery. Leads are secured in the epidural space. The generator is placed under your skin. You’re usually home the same day or next morning.
Recovery is quick, but learning takes time. Most people need 2-4 weeks to get comfortable with programming the device. Around 89% need at least one follow-up with a specialist to tweak settings. It’s not plug-and-play. You have to learn how to use it.
What Can Go Wrong?
Complications aren’t rare. About 1 in 5 people need a revision surgery within two years. The most common issues:
- Lead migration: The wires shift. Pain returns or moves. Happens in 15% of cases.
- Infection: Around 4-7% of implants get infected. Sometimes the whole system has to be removed.
- Battery replacement: Most generators last 5-9 years. Replacing it means another small surgery.
- Insurance hurdles: Even with Medicare coverage, patients often pay $5,000-$10,000 out-of-pocket.
On Reddit’s r/ChronicPain, 41% of negative reviews mention lead migration. One user, PainWarrior89, got 78% relief with a Boston Scientific system-but needed two revisions in 18 months. That’s not failure. It’s reality.
Who Should Avoid It?
SCS isn’t for everyone. Avoid it if you:
- Can’t operate the device (dementia, severe motor impairment)
- Failed the trial stimulation
- Are pregnant
- Have an active infection
- Can’t commit to follow-ups and programming
And if you’re hoping for a miracle? SCS won’t give you that. But for many, it gives something better: the ability to sleep through the night, walk to the mailbox, or hug your grandchild without wincing.

What’s Next for SCS?
The field is moving fast. Boston Scientific’s Evoke® system-still in trials-uses real-time neural feedback to auto-adjust stimulation. It’s like having a smart thermostat for your pain. Early results show 83% of patients had meaningful relief at 12 months.
Medtronic’s Intellis™ 2 adjusts stimulation based on your posture. Stand up? The device knows. Sit down? It changes. That kind of responsiveness is the future.
But the biggest challenge isn’t technology-it’s access. Cost remains a barrier. Insurance approvals take months. Many patients give up before they even try.
Real Outcomes, Real People
On Healthgrades, 82% of 4+ star reviews mention regaining mobility. One patient wrote: “I walked my daughter down the aisle. I hadn’t been able to stand for 10 minutes in 8 years.”
Another: “My monthly opioid bill dropped from $1,200 to $400. I’m not perfect, but I’m present.”
But the same platforms show 3.7-3.9 out of 5 ratings. The complaints? Battery replacements. Lead shifts. Insurance battles. It’s not easy. But for those who made it through, most say it was worth it.
SCS doesn’t promise freedom from pain. It promises a life where pain doesn’t own you.
Is spinal cord stimulation the same as a pacemaker?
They work similarly-both use implanted devices to send electrical signals-but they target different systems. A pacemaker regulates heart rhythm. Spinal cord stimulation blocks pain signals in your nerves. The hardware looks similar, but the purpose and placement are completely different.
Can I get an MRI with a spinal cord stimulator?
It depends on the device. Older models are MRI-unsafe. Newer ones like Boston Scientific’s Precision Montage™ MRI and Medtronic’s Intellis™ are designed to be safe under specific conditions-usually 1.5T or 3.0T scanners, with settings locked by your doctor. Always check with your provider before scheduling an MRI.
How long does the battery last?
Most implantable pulse generators last 5 to 9 years. Some newer models, like Boston Scientific’s WaveWriter Alpha™ Prime, last up to 24 months on high settings. Rechargeable systems can last 10+ years but require daily charging. Your doctor will help you choose based on your pain level and lifestyle.
Will SCS help with back pain?
Yes-if it’s nerve-related. SCS works best for leg pain caused by nerve compression (like sciatica) or failed back surgery syndrome. It’s less effective for pure mechanical back pain from degenerative discs or muscle strain. A trial is the only way to know if it’ll help your specific case.
Does insurance cover spinal cord stimulation?
Medicare covers SCS for approved conditions: failed back surgery syndrome, CRPS, and chronic leg/back pain. Most private insurers follow suit, but pre-authorization is required. Out-of-pocket costs range from $5,000 to $10,000 even with coverage. Always confirm benefits with your insurer before starting the process.
What’s the success rate after 5 years?
About 52% of patients still report significant pain relief at the 5-year mark, according to a 2022 meta-analysis. That’s lower than the 76% seen at 6 months, which suggests some benefit fades over time. But even half of those patients say they’d do it again because their quality of life improved enough to make it worthwhile.
Final Thoughts
If you’ve been living with chronic pain for years, and every option has let you down, spinal cord stimulation might be worth exploring. It’s not a quick fix. It’s not pain-free living. But for many, it’s the bridge between suffering and a life that’s still theirs.

Comments (12)
Ibrahim Yakubu December 5 2025
This is the most comprehensive breakdown of SCS I've ever seen. I've been living with CRPS for 12 years and tried everything - ketamine infusions, nerve blocks, even that weird TENS unit my cousin swore by. The part about the trial phase being non-negotiable? Spot on. I skipped it once because I was desperate. Ended up with a device that felt like a wasp nest in my spine. Never again.
And the battery life? Don't get me started. My 2018 Medtronic unit died after 4 years. Had to pay $8k out of pocket because my insurance called it a 'cosmetic upgrade.' Funny how pain management becomes a luxury when you're too broken to work.
But yeah - I can finally hug my daughter without crying. Worth every scar, every surgery, every fight with the insurance guy.
Don't believe the hype. Do the trial. And if it works? Don't look back.
Brooke Evers December 7 2025
I just want to say how deeply moved I am by the stories in this post - especially the one about walking a daughter down the aisle. I work as a chronic pain coach, and I’ve seen too many people give up because they were told ‘it’s all in your head’ or ‘you’re just getting older.’ But this isn’t about weakness. It’s about biology, about nerves firing wrong, about a body that’s been betrayed by its own wiring.
SCS isn’t magic, but it’s one of the few tools that gives people back agency. The fact that it reduces opioid use by over half? That’s not just clinical data - that’s dignity restored. And yes, the complications are real. Lead migration, infections, insurance nightmares - I’ve sat with people in tears over those. But I’ve also sat with people who, for the first time in years, slept through the night. That’s the balance. That’s the humanity here.
To anyone considering this: don’t rush. Do the trial. Find a specialist who listens. And if you fail the trial? That doesn’t mean you’re broken. It means your pain has its own language - and maybe it’s not ready to be silenced by electricity yet.
You’re not alone. I see you.
Chris Park December 7 2025
Let’s cut through the corporate PR. SCS isn’t a breakthrough - it’s a profit engine. Look at the prices: $45k for a device that fails 20% of the time? And the manufacturers push these ‘new’ models every 2 years like it’s an iPhone update. Boston Scientific? Medtronic? They own the patents, the lobbying, the ‘clinical trials’ funded by their own labs. The 89% success rate? That’s from studies where patients were selected for ideal conditions - no depression, no obesity, no comorbidities. Real-world? More like 40-50%.
And the MRI safety claims? That’s marketing. My cousin had his lead melt during a scan because the ‘safe’ settings weren’t calibrated right. They didn’t even tell him the scanner had to be locked down by the manufacturer’s rep - not his radiologist. This isn’t medicine. It’s a rigged game.
Meanwhile, the real solution - physical therapy, diet, mindfulness - gets buried under layers of tech hype. Why? Because you can’t patent a yoga mat.
Saketh Sai Rachapudi December 7 2025
this is all western nonsense why dont you try ayurveda or yoga or even just stop being weak indian people have been living with pain for centuries without some electric box in their spine you think your pain is special its not just pray more and stop wasting money on american gadgetsjoanne humphreys December 8 2025
I appreciate how thorough this is - especially the breakdown of who qualifies and who doesn’t. I’ve had chronic back pain since a car accident in 2017, and I’ve been through the same cycle: meds, PT, injections, more meds. I did the trial last year and got 60% relief. The implant went in last month. It’s not perfect - I still have bad days - but I can now sit through my son’s soccer games without needing to lie down after five minutes.
What nobody talks about enough is the emotional labor of learning to use the device. It’s not like turning on a light. You have to become a technician. You have to learn what settings work when you’re sitting, standing, walking, even lying on your side. And the follow-ups? They’re not optional. You have to advocate for yourself.
Also - the battery thing. Mine’s rechargeable. I charge it every other night. It’s become part of my routine, like brushing my teeth. Weird, but manageable.
Thank you for writing this. It’s the kind of post that gives people real information, not false hope.
Kumar Shubhranshu December 9 2025
trial is key dont skip itMayur Panchamia December 11 2025
Oh please. You people are so naive. You think these ‘high-frequency’ devices are some miracle? They’re just fancy TENS units with a $40k price tag and a surgeon’s signature on the bill. And let’s not pretend the ‘paresthesia-free’ tech is new - I’ve been using a Chinese knockoff on eBay since 2020 for $200. Same waveform, same results. The only difference? You’re paying for the brand name and the hospital markup.
And don’t even get me started on ‘real-time neural feedback.’ That’s just AI trying to sound smart while the device still randomly shuts off at 3 a.m. My friend’s Evoke prototype? It started vibrating when he sneezed. He had to turn it off with a remote while he was in the shower.
This isn’t innovation. It’s medical theater. The real breakthrough? Learning to live with pain - not outsourcing it to a gadget that needs a recharge and a $10k surgery every 6 years.
Karen Mitchell December 12 2025
While the clinical data presented is statistically compelling, one cannot ignore the ethical implications of promoting a high-cost, invasive intervention for a condition that is, at its core, a manifestation of systemic neglect in chronic pain management. The normalization of surgical solutions for what are often psychosocially mediated phenomena is both medically questionable and economically exploitative.
Furthermore, the assertion that patients with untreated depression are less likely to benefit is not merely a clinical observation - it is a dangerous justification for excluding vulnerable populations from care. Should one’s mental health status determine eligibility for pain relief? This is not medicine. This is triage disguised as innovation.
And let us not forget: the insurance hurdles described are not anomalies - they are the norm. This is not a treatment. It is a privilege.
Rashmi Gupta December 12 2025
Everyone’s acting like this is the first time anyone’s tried shocking the spine. Back in the 90s, my uncle got one of these things after his back surgery. Lasted three months. Then the wires moved. Then the battery died. Then the doctor said ‘maybe it’s just your attitude.’
Same story. Same hype. Same $40k bill. Same ‘you’re lucky you even got approved.’
I’m not saying it doesn’t work for some. But why is this the only option people talk about? Why not talk about why we don’t have better non-invasive options? Why is the solution always ‘cut them open and plug something in’?
It’s not progress. It’s repetition with better marketing.
Andrew Frazier December 13 2025
Bro. I’m not even mad. I’m just disappointed. You spent all this time writing about SCS like it’s some kind of elite tech, but the real story? It’s the same old story: rich people get the new shiny thing, poor people get opioids and silence.
And don’t even get me started on the ‘you need to be mentally stable’ part. So if you’re poor, depressed, and in pain? Tough luck. Go back to your job at Walmart. We’ll wait for you to get a therapist and a credit score before we let you feel human again.
Meanwhile, the guy who invented this tech? He’s got a Tesla and a house in Malibu. The rest of us? We’re still Googling ‘how to survive without sleeping’.
brenda olvera December 13 2025
I’m from a small town in Texas. We don’t have specialists nearby. I had to drive 4 hours just to get the trial approved. My insurance denied it twice. I cried in the parking lot of the clinic. But I kept going. I did the trial. Got the implant. Now I can play with my grandkids again.
This isn’t about being strong or weak. It’s about being heard.
Thank you for writing this. Someone out there needs to read it. Maybe it’ll save them from giving up.
Ibrahim Yakubu December 14 2025
That last comment about the grandkids? That’s why I keep mine on. Even when the battery’s low and the leads are acting up. Even when the insurance rep tells me ‘we can’t cover that revision.’
I didn’t get SCS to be pain-free. I got it so I could hold my granddaughter without flinching. That’s the whole damn point.
And yeah - I still hate the charging. But I’d rather charge a battery than mourn a life.