Buprenorphine Safety Risk Calculator
How Buprenorphine Works
Buprenorphine has a "ceiling effect" that limits respiratory depression even at high doses. However, this protection disappears when mixed with other central nervous system depressants.
Remember: All fatal buprenorphine overdoses involve mixing with other depressants. Never combine with alcohol, benzodiazepines, sleep aids, or other opioids.
When someone is trying to get off opioids, safety isn’t just important-it’s life-or-death. That’s where buprenorphine comes in. Unlike full opioid agonists like methadone or heroin, buprenorphine doesn’t keep getting stronger the more you take. It hits a wall. And that wall? It’s called the ceiling effect. This isn’t just a pharmacology term. It’s what lets people go to work, pick up their kids, or sleep through the night without the crushing risk of overdose that comes with other opioids.
What Is the Ceiling Effect, Really?
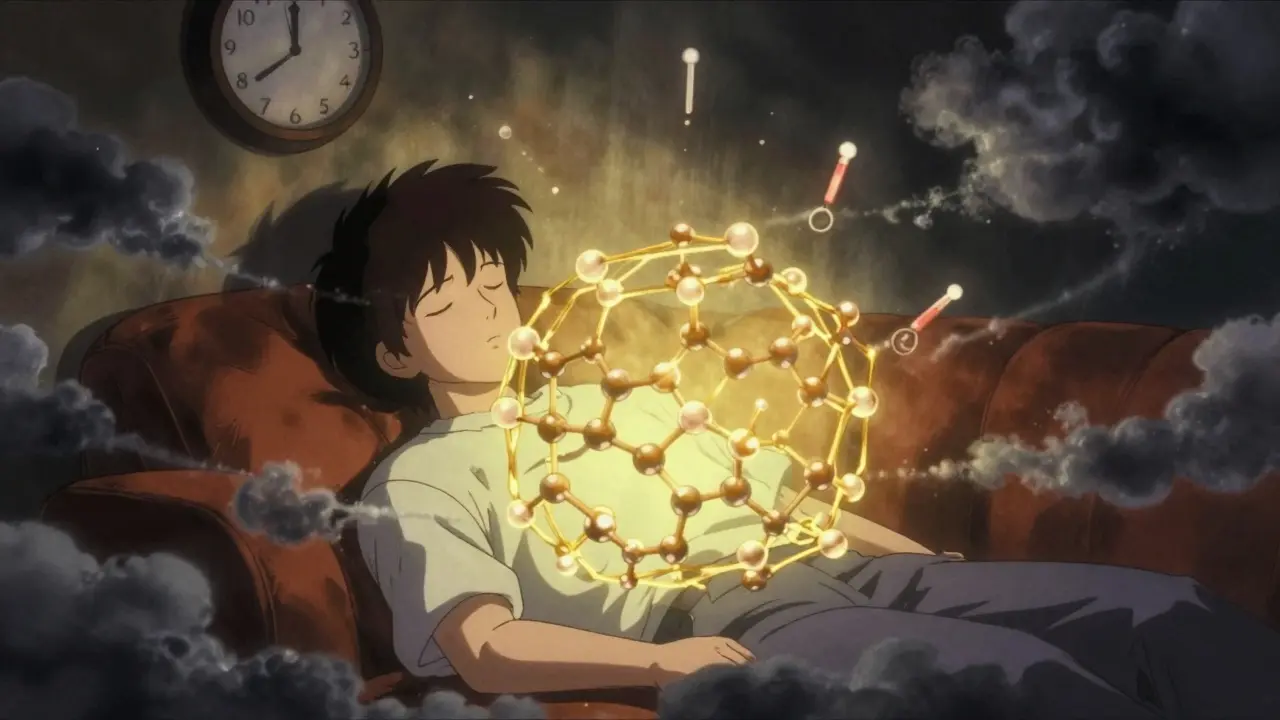
The ceiling effect isn’t magic. It’s science. Buprenorphine binds tightly to the brain’s mu-opioid receptors, but it doesn’t fully turn them on. Think of it like a dimmer switch that only goes up to 60% brightness, no matter how far you turn it. Even if you take 70 mg, the effect on breathing doesn’t get any stronger after about 24 mg. That’s why, in clinical studies, people taking 16 mg a day don’t have more respiratory depression than those taking 8 mg. The same goes for euphoria. You don’t get higher on 24 mg than you do on 16 mg. That’s huge. With heroin or oxycodone, more dose = more high = more danger. With buprenorphine? It plateaus.
This ceiling applies most strongly to respiratory depression-the main cause of opioid overdose deaths. But here’s the nuance: it doesn’t apply to everything. Pain relief? That can still increase with higher doses. That’s why doctors sometimes need to go up to 24 mg for patients with chronic pain and opioid use disorder. The ceiling protects you from dying. It doesn’t mean the drug stops working.
Why Buprenorphine Is Safer Than Methadone
Methadone is effective. But it’s a full agonist. That means its effects keep rising with dose-no ceiling. One study found methadone overdose rates were more than twice as high as buprenorphine’s in treatment programs. Why? Because methadone can easily push someone into dangerous respiratory suppression. Buprenorphine? Even at high doses, it’s far less likely to stop your breathing.
And here’s another advantage: buprenorphine blocks other opioids. If you’re on 16 mg of buprenorphine and someone tries to give you heroin, it won’t work. The buprenorphine is already locked onto the receptors. It’s like a bouncer that won’t let anyone else in. That’s why people on buprenorphine are less likely to relapse-they don’t get the same high, even if they try.
Common Side Effects (And Why They’re Manageable)
No drug is perfect. Buprenorphine has side effects, but they’re usually mild compared to full opioids.
- Headache-reported in about 18% of users during clinical trials. Usually fades after a few days.
- Constipation-affects roughly 12%. Still less than what you’d see with oxycodone or morphine.
- Withdrawal symptoms-if you start buprenorphine too soon after your last opioid, you can get sudden, intense withdrawal. This is called precipitated withdrawal. It happens in about 25% of cases when people don’t wait long enough. The fix? Wait until you’re in mild withdrawal before taking it. Your doctor should guide this.
- Low energy or drowsiness-some people feel a bit foggy at first. Most adapt within a week or two. If you’re still tired after a month, your dose might be too high.
Unlike methadone, buprenorphine doesn’t usually make people feel “stoned.” Many users say they can work, drive, or care for their kids without feeling impaired. One Reddit user put it simply: “I can take my 16mg and go to work without feeling like I’m on something, which methadone never allowed.”
The Real Risk: Mixing With Other Drugs
Buprenorphine’s safety isn’t absolute. It’s conditional. The ceiling effect protects you-until you add something else. A 2022 study found all 18 fatal buprenorphine overdoses between 2019 and 2021 involved mixing with benzodiazepines, alcohol, or other sedatives. That’s the pattern. Not buprenorphine alone. Always. Every time.
If you’re on buprenorphine, avoid:
- Benzodiazepines (Xanax, Valium, Klonopin)
- Alcohol
- Sleep aids (Ambien, Lunesta)
- Other opioids (even “just one hit”)
These combinations shut down breathing faster than buprenorphine ever could on its own. That’s why doctors ask you to list every medication you take-and why some pharmacies now flag buprenorphine prescriptions when someone also fills a benzodiazepine.
Who Might Not Do Well on Buprenorphine?
Buprenorphine works for most people-but not all. Some patients with severe, long-term opioid dependence need higher doses to feel stable. Studies show that people with chronic pain or a history of heavy heroin use often need 16-24 mg daily to stop cravings and withdrawal. At 8 mg, they might still feel sick or anxious.
Also, buprenorphine isn’t always enough on its own. It’s not a cure. It’s a tool. People who pair it with counseling, peer support, or job training have much better long-term outcomes. But even without those supports, buprenorphine still saves lives. The American Society of Addiction Medicine says: don’t wait for perfect conditions to start treatment. Start now.

New Developments: Weekly Injections and Better Access
In 2023, the FDA approved Sublocade-a monthly injection of buprenorphine. No more daily pills. No more risk of missing a dose. Clinical trials showed nearly half of users stayed abstinent for over six months. That’s a big jump from the 35% seen with daily sublingual forms.
And access is getting easier. Since the MAT Act of 2021, doctors no longer need a special X-waiver to prescribe buprenorphine. Any licensed provider can do it. That means more people in rural areas, primary care clinics, and emergency rooms can now offer this life-saving treatment.
How Dosing Works in Practice
Most people start with 2-4 mg on the first day. Doctors increase it slowly-by 2-4 mg every few hours-until withdrawal symptoms stop. The goal? Find the lowest dose that keeps you stable. For most, that’s 8-16 mg daily. Some need up to 24 mg. But going beyond 24 mg? It doesn’t help. And it doesn’t increase risk. That’s the ceiling in action.
It’s not about how much you take. It’s about how well you feel. If you’re not craving opioids, not feeling sick, and not using, you’re on the right dose. Not higher. Not lower.
The Bigger Picture
Over 2.5 million Americans have opioid use disorder. Buprenorphine is now used in about half of all medication-assisted treatments. That’s more than methadone. Why? Because it’s safer, easier to prescribe, and lets people live normally. It doesn’t erase addiction. But it gives you back control.
The ceiling effect isn’t a limitation. It’s the reason buprenorphine works. It’s what lets you stay alive while you heal. It’s why someone can go from using heroin every day to holding a job, reconnecting with family, and sleeping without fear.
This isn’t just a drug. It’s a second chance.
Can you overdose on buprenorphine alone?
Overdosing on buprenorphine alone is extremely rare. Its ceiling effect limits respiratory depression, even at very high doses. In clinical studies, doses up to 70 mg didn’t cause fatal breathing problems in opioid-tolerant individuals. However, overdose is possible in people with no opioid tolerance, such as children or non-users who accidentally ingest it. Fatal cases almost always involve mixing with other depressants like alcohol or benzodiazepines.
Is buprenorphine addictive?
Yes, buprenorphine can cause physical dependence, but it’s not addictive in the way heroin or oxycodone is. People on buprenorphine don’t typically crave it for euphoria. Instead, they use it to avoid withdrawal and cravings for stronger opioids. When taken as prescribed, it reduces the urge to misuse other drugs. Withdrawal symptoms are usually milder than those from full opioids and can be managed with gradual tapering under medical supervision.
How long does it take for buprenorphine to start working?
Buprenorphine starts working within 30 to 60 minutes after sublingual administration. Most patients notice a reduction in cravings and withdrawal symptoms within the first hour. Full stabilization usually takes a few days to a week. The drug’s long half-life means effects last 24 to 36 hours, allowing for once-daily dosing. For some, even three times weekly dosing works, especially with extended-release injections.
Why do some people need higher doses of buprenorphine?
People with severe, long-term opioid dependence often need higher doses-up to 24 mg daily-to fully block cravings and prevent withdrawal. This is especially true for those with chronic pain or a history of heavy heroin use. Buprenorphine’s high receptor affinity means it displaces other opioids, but if the body has built up a high tolerance, a larger dose is needed to occupy enough receptors to stop withdrawal symptoms. Dosing is individualized, and there’s no benefit to exceeding 24 mg daily.
Can you switch from methadone to buprenorphine?
Yes, switching from methadone to buprenorphine is possible and often done for safety or convenience. However, it requires careful planning. You must first reduce your methadone dose to 30 mg or less per day and wait at least 24-48 hours after your last dose before starting buprenorphine. Starting too soon can trigger precipitated withdrawal. A skilled provider will guide the transition, often using low initial buprenorphine doses and titrating slowly.


Comments (10)
Gloria Ricky February 12 2026
i just started buprenorphine last month and honestly? it’s been a game changer. no more waking up in a sweat wondering if i’ll make it to work. i can actually hear my kid laugh now. also, yeah, the headache sucked for like 3 days but then poof. gone. side effects are way overblown if you’re not mixing stuff. stay clean, stay alive.Kristin Jarecki February 12 2026
The pharmacological profile of buprenorphine, as a partial mu-opioid receptor agonist with high affinity and low intrinsic efficacy, confers a distinct safety advantage over full agonists. The ceiling effect on respiratory depression is not merely a clinical observation but a well-documented phenomenon in peer-reviewed literature, particularly in studies utilizing quantitative pharmacokinetic modeling. This mechanism fundamentally alters the risk-benefit calculus in opioid use disorder management.Rachidi Toupé GAGNON February 14 2026
buprenorphine is basically the superhero of addiction meds 🦸♂️💊 no cap. you don’t get blasted, you don’t OD, you just… exist. like a calm version of yourself. i’ve seen people go from ‘i can’t hold a job’ to ‘i’m running a small biz’ on this. the ceiling? it’s not a wall-it’s a safety net.Jim Johnson February 14 2026
i was skeptical at first but after 6 months? this stuff saved my life. i used to do 30 mg of oxycodone a day. now i take 16 mg of suboxone and i’m not even thinking about it. the constipation? yeah, it’s a thing. but i just drink water and eat prunes. no biggie. and the fact that i can drive my kid to school without feeling like a zombie? priceless.Vamsi Krishna February 15 2026
you all are naive. the government is using this to control us. buprenorphine is a gateway to lifelong dependency. they don’t want you cured, they want you compliant. and the ‘ceiling effect’? that’s just marketing. the real danger is the pharmaceutical industry profiting off your addiction. why do you think they pushed this over methadone? because it’s more profitable. think for yourself.Brad Ralph February 16 2026
ceiling effect = nature’s way of saying ‘ chill out bro ’ 😎Pat Mun February 16 2026
i’ve been on buprenorphine for over two years now, and honestly, the biggest shift wasn’t the physical relief-it was the mental space it gave me. before, every thought was consumed by ‘when’s my next dose,’ ‘how do i hide this,’ ‘will i get caught.’ now? i read books. i started painting. i called my mom. i didn’t even realize how much emotional bandwidth i’d lost until it came back. and yeah, i still get sleepy sometimes, but that’s just my body catching up. i used to think recovery meant being perfect. now i know it just means showing up. even on the days you feel like crap. even if you forget to take your pill once. even if you cry during your therapy session. you’re still winning. you’re still here. and that’s everything.Skilken Awe February 18 2026
this article is a glorified pharmaceutical ad. the ‘ceiling effect’ is a myth perpetuated by FDA-approved propaganda. real addicts know: if you take enough, anything can kill you. they downplay the withdrawal because they don’t want you to quit. and don’t get me started on the ‘blocking’ effect-tell that to the guy who got 100 mg of fentanyl and still OD’d. this isn’t treatment. it’s chemical containment.andres az February 19 2026
they’re lying. buprenorphine is a slow poison. it’s in the water supply. the ‘ceiling effect’? that’s just what they tell you so you don’t panic. next they’ll say the moon landing was fake. trust no one. #deepstate #buprenorphineisabrainwashSteve DESTIVELLE February 21 2026
the real question is not whether buprenorphine has a ceiling effect but whether humanity has the moral courage to accept that healing is not a linear path but a spiral of surrender and rediscovery. we mistake medication for cure because we fear the silence that follows the storm. yet in that silence lies the voice we have spent decades drowning out. the drug is not the answer. the answer is the space it creates. and in that space we must choose to listen even when the world screams louder than our own bones