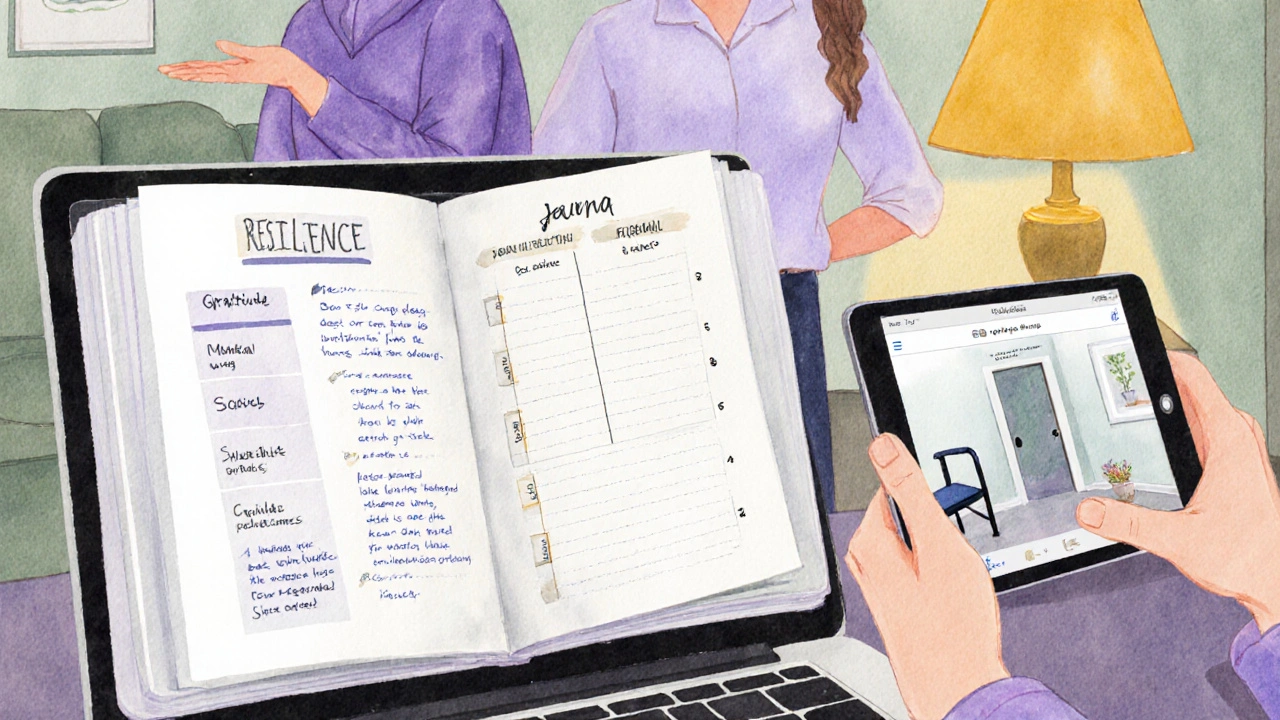
Resilience Building Progress Tracker
Track your progress across the three core resilience pillars:
Select activities you'll complete this week to build resilience:
Reflect on your week:
Quick Take
- Resilience means bouncing back physically, mentally, and socially after setbacks.
- Poor muscle control limits daily tasks and can drain confidence.
- Combining targeted exercise, stress‑relief habits, and a strong support network builds lasting resilience.
- Personalized plans that include building resilience reduce injury risk and improve quality of life.
- Regular check‑ins with therapists keep progress on track.
What "Resilience" Really Is
When we talk about Resilience is a person’s capacity to recover from physical, emotional, or social challenges, we’re not just describing a vague "toughness". In a health context, resilience blends physiological adaptation, mental grit, and social support into a measurable skill set that can be trained.
Why Poor Muscle Control Challenges Resilience
People with poor muscle control often experience involuntary weakness, spasticity, or coordination loss. Conditions such as cerebral palsy, stroke after‑effects, or progressive diseases like ALS fall under the umbrella of neuromuscular disorder any condition that impairs the nerves that control muscle movement. The everyday struggle to stand, grasp, or walk creates a constant feedback loop: failure leads to frustration, which then reduces motivation for rehab, slowing progress further.

Core Strategies for Building Resilience
Resilience isn’t built by a single activity. It’s a trio of physical, mental, and social habits that reinforce each other.
1. Targeted Physical Training
Professional Physical therapy structured, hands‑on treatment that improves strength, balance, and movement patterns remains the cornerstone. Therapists design progressive overload routines that respect the client’s safety limits while nudging the nervous system toward better coordination.
- Start with seated marching or assisted standing to activate core muscles.
- Gradually incorporate resistance bands to challenge weak muscle groups.
- End each session with low‑impact cardio (e.g., recumbent bike) to boost circulation.
For those who can’t safely attend a clinic, Adaptive exercise modifications or assistive tools that let individuals work out despite physical limitations offers a home‑friendly alternative. Think: Velcro‑wrapped ankle weights, grip‑enhancing gloves, or chair‑based rowing machines.
2. Mental Toughness and Stress Management
Repeated setbacks can shrink confidence. Integrating Stress management techniques that lower cortisol and improve emotional regulation helps the brain stay receptive to new motor patterns.
- Practice guided breathing for 5 minutes before each therapy session.
- Use a simple gratitude journal: note three successes, however tiny, each day.
- Consider mindfulness apps that offer short, movement‑linked meditations.
These habits lower the physiological “fight‑or‑flight” response, allowing neuroplasticity the brain’s ability to rewire itself in response to practice and experience to occur more efficiently.
3. Social Support Networks
Isolation magnifies frustration. Connecting with family, peers, or support groups adds an emotional safety net and supplies practical tips.
- Schedule weekly check‑ins with a trusted friend who can help track progress.
- Join online forums for people with similar neuromuscular challenges; shared stories often spark new exercise ideas.
- Invite an Occupational therapist a specialist who helps people perform daily activities safely and efficiently to assess home layouts and recommend adaptive tools (grab bars, widened doorways, etc.).
Designing a Personalized Resilience Plan
One‑size‑fits‑all rarely works when muscle control is compromised. Follow these steps to craft a plan that sticks.
- Assess baseline abilities. Work with a physical therapist to record range of motion, strength grades, and functional tasks (e.g., rising from a chair).
- Set micro‑goals. Instead of “walk unaided,” aim for “stand for 30 seconds with a cane three times a day.”
- Choose the right mix of activities. Pair a 10‑minute adaptive exercise routine with a 5‑minute mindfulness session.
- Schedule regular reviews. Every two weeks, revisit goals, tweak intensity, and celebrate milestones.
- Document progress. Use a simple spreadsheet: date, activity, perceived effort, any pain, and mood rating.
Consistency beats intensity. A daily 15‑minute commitment yields more neural rewiring than a sporadic hour‑long marathon.
Common Pitfalls and How to Dodge Them
- Skipping warm‑ups. Jumping straight into strength work spikes injury risk. A 5‑minute gentle range‑of‑motion routine prepares muscles and nerves.
- Over‑relying on pain as a metric. Some discomfort signals progress, but sharp or shooting pain indicates a red flag. Learn the difference early.
- Neglecting mental rest. Burnout isn’t limited to work; repetitive rehab without mental breaks can erode motivation.
- Isolating the journey. Going it alone removes accountability. Invite a friend to attend one therapy session per month.
- Setting unrealistic goals. If the target is far beyond current capacity, frustration builds. Break big aims into bite‑sized, measurable steps.
Resources & Professional Support
Below is a quick reference that matches common needs with the right expert or tool.
| Need | Professional / Tool | Typical Frequency |
|---|---|---|
| Strength & Mobility | Physical therapist | 1‑2 sessions/week |
| Daily Living Skills | Occupational therapist | Monthly check‑in |
| Mind‑Body Balance | Guided meditation apps (e.g., Insight Timer) | 5‑10min/day |
| Community Support | Online peer groups (e.g., Muscular Dystrophy Association forums) | Weekly participation |
| Progress Tracking | Simple spreadsheet or rehab journal | After each session |
Frequently Asked Questions
Can resilience be measured objectively?
Yes. Clinicians use standardized scales such as the Functional Independence Measure (FIM) for daily tasks and the Berg Balance Scale for mobility. Combining these scores with self‑reported confidence ratings gives a rounded picture of resilience progress.
How soon can I expect noticeable improvements?
Most people notice subtle gains-like holding a cup longer or feeling less breathless-within 4‑6 weeks of consistent, low‑intensity training. Larger functional milestones (e.g., walking 10meters unaided) often take 3‑6 months, depending on the severity of the underlying condition.
Is it safe to combine strength work with cardio?
When supervised by a therapist, yes. Alternating days-strength on Monday, cardio on Tuesday-prevents over‑fatigue and promotes both muscular and cardiovascular health, which together boost overall resilience.
What role does nutrition play?
Protein supports muscle repair, while omega‑3 fatty acids aid nerve health. A balanced diet rich in fruits, vegetables, lean meats, and whole grains complements physical rehab and helps maintain energy levels for daily challenges.
Do I need expensive equipment?
No. Many adaptive exercises rely on household items: water bottles for weight, sturdy chairs for support, and resistance bands that cost under $20. The key is consistency, not how fancy the tools are.


Comments (13)
carol messum October 2 2025
Reading through the post really made me think about how resilience is more than just toughening up; it's about finding ways to keep moving even when muscles don’t cooperate the way we want. For folks with poor muscle control, every little victory-like standing for ten seconds-feels huge. Building resilience gives them a mental cushion that helps them stay motivated despite setbacks. It also creates a habit loop where effort leads to small improvements, which then fuels confidence. Over time those confidence boosts can translate into real functional gains because the brain starts trusting the body again. So, resilience is basically the glue that holds the physical and emotional parts together.
Jennifer Ramos October 13 2025
Thanks for sharing such a thorough guide! The mix of physical, mental, and social tips really covers all the bases. 😊 I especially love the idea of gratitude journaling-simple but powerful. Keep up the great work!
Grover Walters October 24 2025
While the article presents a commendable overview, it is essential to contextualize resilience within the broader framework of neuroplastic adaptation and motor learning theory. Resilience, in the clinical sense, should not be conflated with mere perseverance; it is a measurable construct that reflects the capacity of the central nervous system to reorganize in response to repetitive, task‑specific stimuli. Empirical studies indicate that progressive overload, even when modest, can induce synaptic strengthening, thereby improving motor unit recruitment patterns in individuals with compromised proprioception. Moreover, the integration of mental toughness techniques, such as structured mindfulness, has been shown to modulate cortical excitability, facilitating more efficient neuro‑rehabilitation outcomes. It is also critical to recognize the role of affective support; social isolation can exacerbate maladaptive neuro‑chemical cascades, hindering motor relearning. Therefore, an interdisciplinary approach that synthesizes physiotherapy, occupational therapy, and psychosocial interventions is not optional but indispensable. The article’s suggested weekly goals provide a useful scaffold, yet they must be personalized based on baseline functional assessments such as the Berg Balance Scale and the Functional Independence Measure. In practice, clinicians ought to employ iterative goal‑setting, periodically revisiting and recalibrating targets in accordance with observed progress and patient-reported outcome measures. Finally, adherence remains the linchpin of any resilience‑building program; without consistent engagement, the hypothesized neuro‑plastic benefits will remain theoretical. In sum, while the guide offers an entry point, practitioners should augment it with evidence‑based protocols tailored to the individual’s neurological profile.
Amy Collins November 4 2025
Nice overview, but the jargon about "progressive overload" feels over‑engineered for home users. Most people just need simple, repeatable moves, not a PhD‑level prescription.
amanda luize November 14 2025
Honestly, the whole "resilience" hype is a distraction pushed by big pharma and tech giants seeking data on vulnerable populations. They want to sell you apps, wearables, and supplements while ignoring the root cause: systemic neglect of neuro‑disorders. Don’t be fooled by glossy progress bars.
Chris Morgan November 25 2025
All this positivity ignores the harsh reality that many will never regain full function; optimism alone won’t fix broken nerves.
Pallavi G December 6 2025
Hey everyone! Let’s keep the momentum going. Small steps like a 5‑minute seated march every morning can add up, and celebrating those wins fuels confidence. If you feel stuck, try pairing the exercise with a favorite song – the rhythm can help your body sync up. Remember, you’re not alone; share your progress in the comments so we can cheer each other on! 🌟
Rafael Lopez December 17 2025
Indeed, consistency is key, and to maximize benefits, consider integrating a brief warm‑up, followed by targeted resistance band work, then a cooldown that incorporates deep breathing; this sequence not only prepares the musculoskeletal system, but also primes the autonomic nervous system, reducing stress hormones, and enhancing neuroplastic potential. Additionally, tracking metrics such as perceived exertion, pain levels, and mood after each session can provide valuable feedback for adjusting intensity, ensuring steady progression without overtraining.
Craig Mascarenhas December 28 2025
Looks like another push from the “wellness industry” to get us hooked on gadgets. Remember, most of these tools are designed to harvest data, not to truly help. Stay skeptical.
aarsha jayan January 8 2026
Great points! I’d add that fostering a community-whether online or in‑person-creates a safe space where members can exchange tips, celebrate milestones, and provide emotional backup during tough days. Inclusivity matters; everyone’s journey is unique, and hearing diverse stories can inspire new strategies.
Rita Joseph January 19 2026
Building on that, it’s useful to maintain a simple log: date, activity, duration, and a quick self‑rating of effort and mood. Over weeks, patterns emerge, highlighting what works best for you. For example, you might notice that breathing exercises before therapy boost focus, while a midday walk improves stamina. Such data-driven tweaks turn a generic plan into a personalized roadmap.
abhi sharma January 29 2026
Wow, groundbreaking advice-just do the stuff you already know.
mas aly February 9 2026
I appreciate all the perspectives shared here. It’s clear that resilience isn’t a one‑size‑fits‑all concept; it blends physical effort, mental framing, and social connection. If anyone feels overwhelmed, start with the smallest doable task-perhaps a single stretch-and gradually layer in the other components. Over time, those tiny actions compound into meaningful progress.