When a drug sends your body into crisis-hives swelling shut, skin peeling off, or your lungs shutting down-it’s natural to want to avoid every similar medication forever. But not all reactions mean you need to ban an entire drug family. Some are harmless flukes. Others are life-threatening red flags. Knowing the difference could save you from unnecessary suffering-or worse, a second near-fatal reaction.
Not All Drug Reactions Are Allergies
Most people think a rash or upset stomach after taking a pill means they’re "allergic." But true drug allergies? They’re rare. Only about 10-15% of reported reactions are immune-driven. The rest? They’re side effects. Predictable. Dose-related. Not dangerous in the same way.Take amoxicillin. Around 5-10% of people get a non-itchy, flat rash after taking it. It’s common. It’s not an allergy. It doesn’t mean you can’t take penicillin, cephalosporins, or other beta-lactams later. But if you break out in hives, swell up, or struggle to breathe within minutes? That’s IgE-mediated anaphylaxis. That’s a red flag for the whole class.
Here’s the problem: most doctors don’t dig deep enough. A 2021 study found that only 28% of electronic health records include enough detail to tell if a reaction was truly allergic. So if you said "I got a rash," and the system logged "Penicillin Allergy," that’s it. You’re blocked from everything in that family-even if you never had a real allergy.
These Drug Families Demand Total Avoidance
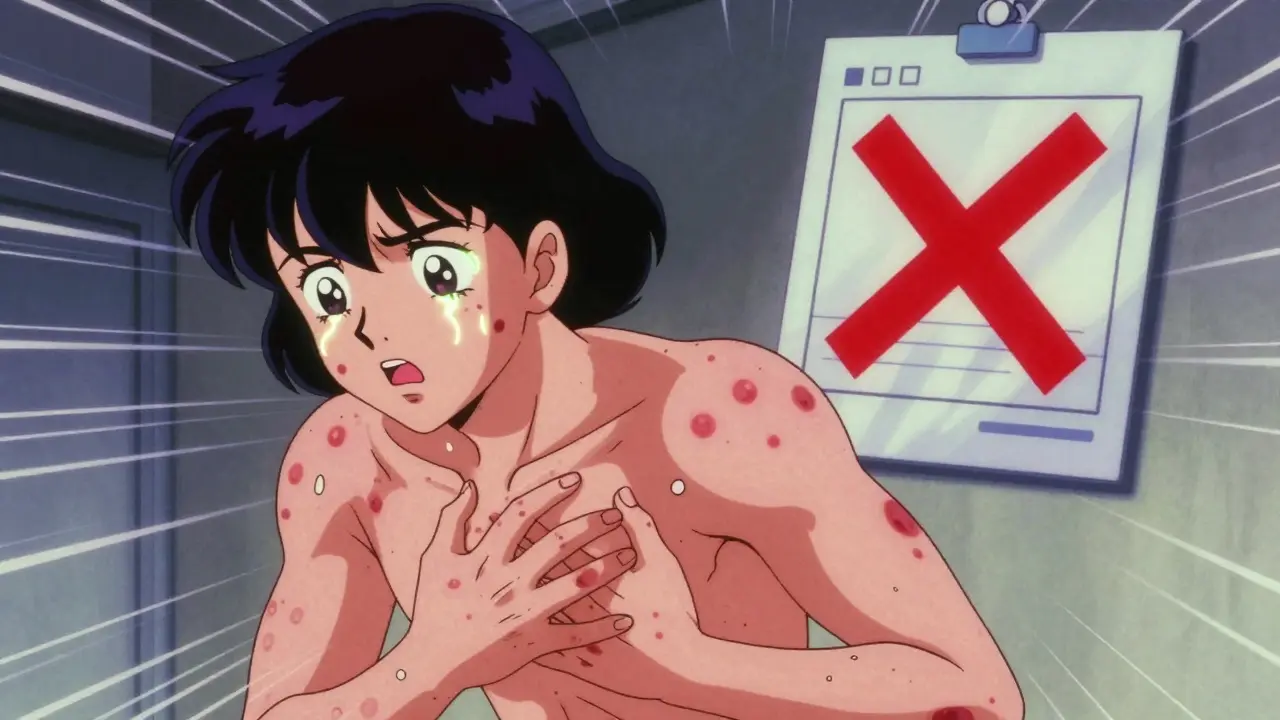
Some reactions are so severe, so unpredictable, that avoiding the entire class isn’t just smart-it’s life-saving.Sulfa antibiotics like Bactrim or Septra can trigger Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN). TEN kills 30-50% of people who get it. If you’ve had either, you must avoid all sulfonamide antibiotics. Cross-reactivity here is real. Even if the next sulfa drug is "different," your immune system remembers.
Anticonvulsants like carbamazepine, phenytoin, and lamotrigine? They’re linked to DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms). This isn’t a rash. It’s your organs failing-liver, kidneys, lungs. Once you’ve had DRESS from one, you’re at high risk for it with others in the same class. Avoidance is permanent.
NSAIDs like aspirin or ibuprofen? If you have aspirin-exacerbated respiratory disease (AERD), you’ll get wheezing, nasal polyps, and asthma attacks when you take any NSAID. About 70% of people with this condition react to all of them. No exceptions. No "try a different one." You need COX-2 inhibitors like celecoxib-or better yet, non-NSAID pain relief.
And then there’s abacavir, an HIV drug. If you carry the HLA-B*57:01 gene variant, taking abacavir can trigger a deadly hypersensitivity reaction. But here’s the twist: genetic testing now exists. If you test negative, you can take it safely. That’s precision medicine in action.
When Avoidance Isn’t Needed-And Could Hurt You
Too many people live with "allergy" labels that aren’t real. And it’s costing them.Over 90% of people labeled "penicillin allergic" aren’t actually allergic. A 2020 Harvard study found that 95% of them can safely take penicillin after proper testing. Why? Because most reactions were rashes from viruses, not drugs. Or they outgrew the allergy. Or they were misdiagnosed as kids.
But because of that label, they’re put on broader-spectrum antibiotics like vancomycin or clindamycin. Those drugs are more expensive. More likely to cause C. diff infections. More likely to contribute to antibiotic resistance. One patient in Sheffield told me she got a severe UTI and was given a week of IV antibiotics because she was "allergic to penicillin." She’d had a mild rash at age 7-no anaphylaxis. After skin testing, she was cleared. Next time? She got amoxicillin. Done in three days.
Same goes for statins. If you got muscle pain on one, you don’t need to avoid all of them. Cross-reactivity? Only 10-15%. Switching to a different statin often works. The same goes for some antidepressants, antivirals, and even chemotherapy drugs.
How to Know What to Avoid
Don’t guess. Don’t rely on a 20-year-old chart note. Ask yourself:- What happened? Was it a rash? Hives? Swelling? Trouble breathing? Low blood pressure? Organ failure? The more severe and systemic, the higher the risk.
- When did it happen? Did it hit within minutes? That’s classic allergy. Days later? Could be DRESS or SJS. Weeks later? Might be a delayed immune response.
- How was it treated? Did you need epinephrine? ICU? Skin grafts? If yes, avoid the whole class.
- Was it confirmed? Did you get skin testing? Blood tests? Genetic screening? If not, you might be avoiding something you don’t need to.
For low-risk reactions-like a mild, non-itchy rash-you might not need to avoid the whole family. For high-risk ones-any reaction that needed hospitalization or caused organ damage-avoidance is almost always required.
The Power of Testing and De-Labeling
There’s a quiet revolution happening in allergy clinics. It’s called de-labeling.Instead of assuming a label is permanent, doctors are now offering:
- Drug skin tests (for penicillins, cephalosporins)
- Oral drug challenges under supervision
- Genetic screening (for abacavir, carbamazepine)
- Component-resolved diagnostics (new blood tests that pinpoint exact allergens)
In 2022, the FDA approved a new test that cuts false positives from 40% down to 11%. That’s huge. And in academic hospitals, 87% now have formal penicillin allergy clinics. Success rates? Up to 85% of patients cleared after testing can safely take the drug again.
One woman in Sheffield had been avoiding all antibiotics since age 12 after a "rash" on amoxicillin. At 48, she got a kidney infection. Her doctor insisted on IV drugs. She pushed back. Got tested. Turned out she had zero IgE antibodies. Took oral amoxicillin. Left the hospital in two days.
What You Should Do Next
If you’ve had a severe reaction:- Get your reaction documented properly: date, drug, symptoms, treatment needed.
- Ask if it was a true allergy-or a side effect.
- Request a referral to an allergist if you’ve been labeled allergic to penicillin, sulfa, or NSAIDs.
- Ask about genetic testing if you’ve had a reaction to anticonvulsants or abacavir.
- Carry a medical alert card or bracelet if you’re truly allergic to a class.
And if you’re a caregiver or clinician: don’t accept vague labels. Push for detail. Push for testing. Because avoiding a whole drug family isn’t just about safety-it’s about access. You might be denying someone the safest, cheapest, most effective drug they’ve ever needed.
If I had a rash from one antibiotic, do I need to avoid all antibiotics?
No. Most rashes from antibiotics like amoxicillin are not allergic. They’re viral rashes or non-allergic side effects. Only if you had hives, swelling, trouble breathing, or needed epinephrine should you avoid the entire class. Even then, testing can often clear you.
Can I outgrow a drug allergy?
Yes. Up to 80% of people who had a penicillin allergy as a child lose it over time. The immune system forgets. That’s why testing later in life is so important. Never assume an allergy is permanent without confirmation.
Are there tests to confirm a drug allergy?
Yes. Skin tests work well for penicillin and some cephalosporins. Blood tests (like ImmunoCap) are improving for other drugs. Genetic tests exist for abacavir and carbamazepine. Oral drug challenges under medical supervision are the gold standard for many reactions. They’re safe and accurate.
Why do doctors avoid entire drug classes after one reaction?
It’s often out of caution, not science. Many doctors don’t have time to dig into reaction details. Electronic health records push automatic alerts. But studies show 32% of these avoidances are inappropriate. Better documentation and allergy referrals can fix this.
What if I need a drug I’m "allergic" to?
Don’t refuse it blindly. Talk to an allergist. Many patients who are labeled allergic can safely take the drug after testing or a supervised challenge. For life-threatening infections, desensitization protocols exist-even for penicillin. You’re not stuck without options.

Comments (1)
Brenda K. Wolfgram Moore February 17 2026
Finally someone breaks this down without sugarcoating. I work in ER and see this daily-patients denied penicillin because of a rash at age 5, then end up on vancomycin for a UTI and get C. diff. The system is broken. Testing isn’t optional-it’s standard of care. Stop letting EHRs make decisions for us.
Also, statin myopathy? Same story. One guy avoided all statins for 12 years after a muscle ache on simvastatin. Switched to rosuvastatin. LDL dropped 40%. No pain. Simple.
Doctors need to stop treating drug reactions like tarot cards.
And yes, I’m the one who pushed the hospital to start a penicillin allergy clinic last year. Took six months of begging. Worth it.