When you're on a blood thinner like warfarin, your life doesn't revolve around pills - it revolves around a number: your INR. It's not just a lab result. It's the difference between staying safe and facing a stroke, or between avoiding a bleed and ending up in the hospital. This number tells your body whether your blood is thin enough to stop clots but not so thin that it won't stop bleeding. And getting it right? That’s the daily job of managing your anticoagulation therapy.
What Is INR, Really?
INR stands for International Normalized Ratio. It’s a standardized way to measure how long it takes your blood to clot. The test starts with a simple blood draw or finger prick, and the lab checks how long it takes for your plasma to form a clot after adding a substance that triggers clotting. That time is called the prothrombin time (PT). But here’s the catch: every lab uses slightly different chemicals. Without standardization, a PT of 15 seconds in one place could mean something totally different in another.
The INR fixes that. It uses a formula that adjusts your PT result based on the sensitivity of the reagent used in the test. That’s why a 2.5 INR means the same thing whether you’re tested in Sheffield, London, or New York. For someone not on blood thinners, a normal INR is 1.0. For people taking warfarin, the target range is usually between 2.0 and 3.0. But that’s not one-size-fits-all. If you have a mechanical heart valve, especially in the mitral position, your target might be higher - 2.5 to 3.5. For atrial fibrillation or a past blood clot, 2.0 to 3.0 is typical.
Why Does the Range Matter So Much?
Think of your INR like a tightrope. Too low, and clots can form - leading to strokes, heart attacks, or pulmonary embolisms. Too high, and you risk bleeding inside your brain, gut, or joints. A 2019 study in JAMA Internal Medicine found that every 0.5-point increase above 3.0 raises your risk of major bleeding by 27%. On the flip side, keeping your INR within target reduces stroke risk by 42% in people with atrial fibrillation, according to the American Heart Association.
It’s not just about hitting the number once. It’s about staying there. The metric that matters most is called time in therapeutic range (TTR). If you’re in your target range 70% of the time, your risk of complications drops sharply. Hospitals with TTR above 65% see 42% fewer strokes and clots than those below 50%. That’s why your doctor doesn’t just want your last INR - they want to see your trend.
Home Testing: Convenience or Necessity?
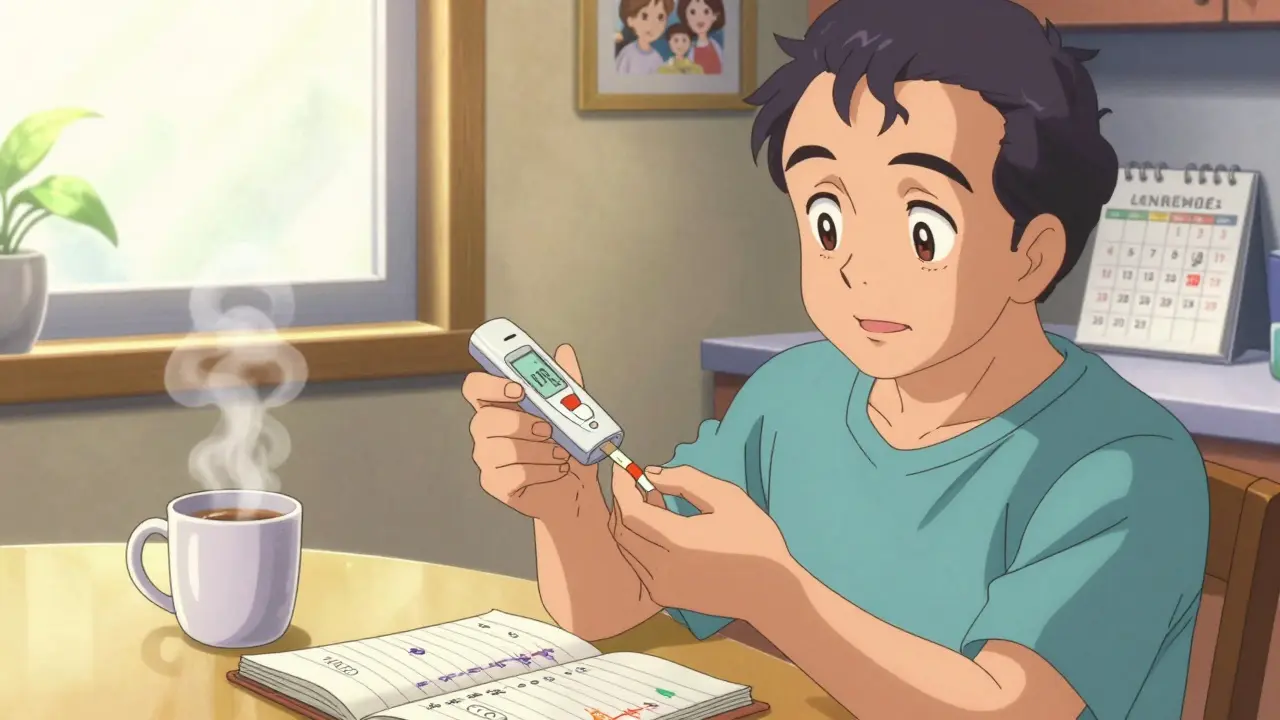
For many, going to the clinic every week or two isn’t just inconvenient - it’s unsustainable. That’s where home INR testing comes in. Devices like the Roche CoaguChek or Abbott Acelis let you prick your finger, place a tiny drop of blood on a strip, and get a result in under a minute. These devices are FDA-approved and accurate enough for clinical use, especially when used correctly.
Studies show people who test at home spend 72% of their time in target range, compared to 58% for those relying on clinic visits. That translates to 34% fewer clots and 21% fewer major bleeds. For someone with a mechanical valve, this isn’t just a convenience - it’s a safety net. One patient in Sheffield told me, “I used to miss appointments because of bus schedules. Now I test on my kitchen table before coffee.”
But home testing isn’t for everyone. If you have shaky hands, poor eyesight, or memory issues, it can be risky. The FDA found that 25-30% of older adults struggle with the technique. And even if you can use the device, insurance coverage isn’t guaranteed. Medicare covers 100% for eligible patients, but private insurers often require prior authorization. Some patients report initial denials - and having to get their doctor to appeal.

Warfarin vs. Newer Blood Thinners
It’s easy to think warfarin is outdated. After all, newer drugs like apixaban, rivaroxaban, and dabigatran don’t require INR checks. They’re simpler. You take them once or twice a day, no blood tests, no dietary restrictions. And they’re just as good - or better - at preventing strokes.
But here’s the catch: warfarin is still the only option for people with mechanical heart valves. It’s also the only choice if you have severe kidney disease. And cost? Warfarin costs about $4 a month. The newer drugs? $550 to $650. That’s a massive difference, especially if you’re paying out of pocket.
That’s why, even in 2026, warfarin isn’t disappearing. About 3.2 million Americans still take it. And while DOACs now make up 70% of new prescriptions, warfarin holds steady in 30% of ongoing cases - mostly because it’s the only tool that works for certain conditions.
What to Do When Your INR Is Off
Your INR isn’t always going to be perfect. Maybe you ate a big plate of kale. Maybe you got sick and skipped a dose. Maybe your device gave a weird reading. Here’s what to do:
- INR below 1.5: Your blood is too thick. You’re at risk for clots. Contact your provider immediately. You may need a dose increase.
- INR between 3.0 and 4.9: You’re in the danger zone. Don’t take your next warfarin dose. Call your doctor. They might advise holding the drug for a day or two, or lowering the dose.
- INR above 5.0: This is an emergency. Major bleeding risk spikes. Stop warfarin. Get medical help within 24 hours. You may need vitamin K or a plasma transfusion.
Never adjust your dose on your own - even if you think you know what you’re doing. A 0.5-point change can mean the difference between safety and crisis.

Testing Tips That Actually Help
Getting reliable INR results isn’t just about the device. It’s about how you do it.
- Test at the same time every day - ideally between 8 a.m. and noon.
- Fasting for 4-6 hours before testing helps reduce variability. No need for a full fast, but skip the greasy breakfast.
- Keep your hand warm before pricking. Cold fingers mean poor blood flow. Rub your hand or run it under warm water.
- Don’t squeeze your finger too hard. That can mix in tissue fluid and mess up the result.
- Record every result - even the weird ones. Apps or paper logs help your doctor spot patterns.
Training matters too. Most home testing programs require 2-4 supervised sessions. Don’t skip them. Even experienced users make mistakes - like using expired strips or not calibrating the device.
The Bigger Picture: Access and Equity
Home INR testing is a game-changer - but not everyone can get it. Rural areas in the UK and US have far fewer anticoagulation clinics. Only 35% of rural healthcare centers offer full INR management, compared to 82% in cities. That means people in villages or remote towns are more likely to be stuck with infrequent testing - and higher risk.
Age also plays a role. Patients over 65 report lower satisfaction with home devices, mostly because of vision or dexterity problems. For them, clinic visits or telehealth support may be better. And while Medicare covers home testing, private insurers vary wildly. Some require co-pays, others won’t cover it at all unless you’ve failed clinic monitoring first.
There’s also a new tech wave: smartphone-connected INR devices. The Bayer CoaguChek ProConnect, approved in early 2023, automatically sends results to your doctor’s system. Accuracy? 98.7% in trials. But it’s still expensive, and not yet widely available on the NHS.
What’s Next for INR Monitoring?
AI is starting to help. Platforms like INR Advisor use machine learning to predict the right warfarin dose based on your history, diet, and other meds. In a Mayo Clinic trial, it was 83% accurate - better than most human clinicians at predicting adjustments.
But the future isn’t just about better tech. It’s about better access. The American College of Chest Physicians now recommends home testing as first-line for all eligible patients. That’s a big shift. And with the global INR monitoring market expected to hit $2.14 billion by 2028, innovation won’t stop.
Still, the core truth remains: INR monitoring isn’t optional. It’s the anchor of safe anticoagulation. Whether you test at home, at a clinic, or through a telehealth visit, your number is your lifeline. Keep it tracked. Keep it honest. And never ignore a result that’s out of range.
What is a normal INR level for someone not on blood thinners?
For someone not taking anticoagulants, a normal INR is 1.0. This means their blood clots at the standard rate. Any reading significantly above or below this suggests a clotting disorder or liver disease, and should be evaluated by a doctor.
Can I check my INR at home?
Yes, home INR testing is safe and accurate for many patients using FDA-approved devices like the Roche CoaguChek or Abbott Acelis. These require a finger prick and give results in under a minute. Training is required, and insurance coverage varies. It’s not recommended for people with poor vision, tremors, or cognitive issues.
Why does my INR change even if I take the same warfarin dose?
Many factors affect INR: diet (especially vitamin K-rich foods like spinach or broccoli), alcohol, illness, other medications (including antibiotics and painkillers), and even changes in your metabolism. That’s why regular testing is essential - your dose isn’t static, even if your routine is.
What should I do if my INR is too high?
If your INR is above 5.0, stop taking warfarin and contact your doctor immediately. For INR between 3.0 and 4.9, skip your next dose and call your provider for guidance. Never adjust your dose without medical advice - high INR increases bleeding risk significantly.
Are newer blood thinners better than warfarin?
For many people, yes - newer drugs like apixaban and rivaroxaban don’t require INR monitoring and have fewer food interactions. But warfarin is still the only option for people with mechanical heart valves or severe kidney disease. It’s also much cheaper. The best choice depends on your condition, cost, and ability to manage regular testing.
How often should I get my INR checked?
When you first start warfarin, you may need testing twice a week. Once stable, most people test monthly. If you’re on home testing and your INR is steady, you might go even longer - but never skip testing without your doctor’s approval. Stable patients rarely need weekly tests - unnecessary testing is common and doesn’t improve outcomes.

Comments (12)
Darren Gormley January 31 2026
INR 2.5-3.5 for mitral valves? 🤔 Bro, I’ve been on warfarin for 8 years and my cardiologist just said ‘whatever your INR is, just don’t let it hit 4.5 or you’ll bleed out like a faucet.’ 😅 I don’t even know what ‘target range’ means anymore. Just gimme the pill and let me live.Mike Rose February 1 2026
why do u need to test so much? i just take my pill and forget about it. my doc says if i dont die in 3 months then im good. lolRuss Kelemen February 3 2026
There’s something beautiful about how something so technical - a number on a screen - becomes the quiet heartbeat of your survival. You don’t think about it until you’re holding that tiny drop of blood on a strip, wondering if today’s the day it flips. But that’s the thing: it’s not about the device, or the cost, or the insurance. It’s about showing up for yourself, every single day. Even when you’re tired. Even when you don’t feel like it. That’s the real therapy.Diksha Srivastava February 3 2026
OMG this post made me cry 😭 I’ve been on warfarin since my heart surgery and I used to hate testing but now I see it as my little daily ritual - like tea and quiet time. You’re not just managing a number, you’re honoring your body. Keep going, warriors! 💪❤️Sidhanth SY February 4 2026
Honestly, home testing is a game changer. My uncle in Delhi couldn’t get to the hospital twice a week - bus schedules, traffic, no transport. Got him a CoaguChek last year. Now he tests every Sunday with his chai. INR stable for 14 months. Tech isn’t magic, but access? That’s the real win.Adarsh Uttral February 5 2026
so like... if i eat a salad every day does my inr go down? i thought it was just about the warfarin dose. also why do they make the strips so expensive??Sheila Garfield February 6 2026
I’ve been doing home testing for 5 years. The biggest mistake I see? People panic when the number jumps 0.3. But it’s not a test score - it’s a trend. I keep a spreadsheet. I log everything: stress, sleep, that weird Thai food I ate. My doctor says I’m the most consistent patient she’s ever had. Not because I’m perfect - because I’m honest.Shawn Peck February 6 2026
DOACS are the future. Warfarin is a 1950s relic. Why are we still making people poke their fingers like cavemen? The new drugs are safer, easier, and honestly - if you can’t afford them, that’s a problem with the system, not your fault. Stop glorifying outdated tech. #ModernMedicineSarah Blevins February 7 2026
The assertion that home INR monitoring improves TTR by 14% is statistically significant (p<0.01) in multiple RCTs, yet the meta-analysis by Patel et al. (2021) noted significant heterogeneity in adherence metrics across socioeconomic strata. Further, the FDA’s 2022 safety alert regarding misapplication in geriatric populations warrants cautious interpretation of generalized efficacy claims.Jason Xin February 9 2026
You know what’s wild? People act like warfarin is some ancient curse. Meanwhile, I’ve got a cousin who’s on Eliquis and he’s out hiking in Patagonia like it’s nothing. Meanwhile I’m sitting here with a logbook and a finger full of bandaids. But hey - at least my pills cost $4. So… win? 🤷♂️Yanaton Whittaker February 9 2026
AMERICA IS THE ONLY COUNTRY THAT STILL LETS PEOPLE USE WARFARIN LIKE IT’S 1987. We have robots that can fly to Mars but you can’t get a simple blood thinner without a blood test? 😭 This is why the world thinks we’re backwards. Get with the program, USA. #DOACs4LifeKathleen Riley February 10 2026
The epistemological underpinnings of INR monitoring reveal a profound ontological tension between quantified selfhood and embodied medical authority. In reducing the complex phenomenology of coagulation to a singular numerical abstraction, we inadvertently reify clinical power structures, wherein the patient becomes a passive conduit for algorithmic governance. The true therapeutic horizon lies not in device accessibility, but in the dissolution of the diagnostic hierarchy - wherein the patient’s lived experience is granted equal epistemic weight to the laboratory result.