It’s easy to assume that if a doctor prescribes a medication, it’s automatically safe. But some common drugs can trigger dangerous heart rhythm problems - even in people who’ve never had heart issues before. Drug-induced arrhythmias aren’t rare. Over 400 medications, from antibiotics to antidepressants, can mess with your heart’s electrical system. And while many cases are mild, others can lead to fainting, hospitalization, or even sudden cardiac arrest.
What Exactly Is a Drug-Induced Arrhythmia?
An arrhythmia is when your heart beats too fast, too slow, or irregularly. When it’s caused by a medication, it’s called a drug-induced arrhythmia. These aren’t random glitches. They happen because the drug interferes with the tiny electrical signals that control your heartbeat. The most common way this occurs is by prolonging the QT interval on an ECG - a measure of how long it takes your heart’s ventricles to recharge between beats. A longer QT interval increases the risk of a life-threatening rhythm called torsades de pointes.
It’s not just the obvious suspects. You might not think your allergy pill or stomach medicine could affect your heart, but antihistamines like diphenhydramine and anti-nausea drugs like ondansetron are on the list. Even some cholesterol-lowering drugs and diabetes medications have been linked to rhythm disturbances. And here’s the twist: some drugs used to treat arrhythmias - like flecainide or amiodarone - can actually cause them in 5-10% of patients. That’s called proarrhythmia, and it’s one of the most dangerous paradoxes in medicine.
Which Medications Are Most Likely to Cause Problems?
Not all drugs carry the same risk. Some are far more dangerous than others, especially when combined. Here are the top culprits based on real-world data:
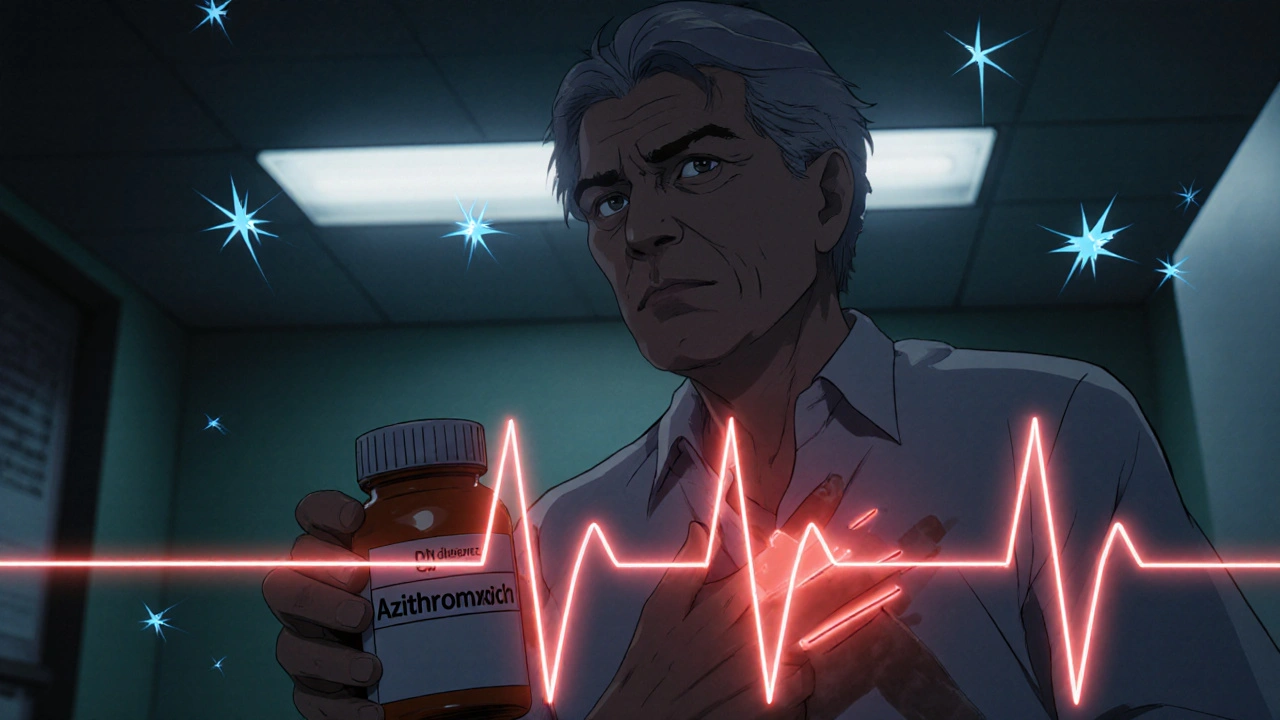
- Antibiotics: Macrolides like azithromycin and fluoroquinolones like levofloxacin prolong the QT interval in 3-5% of users, with the highest risk in the first week of use.
- Antidepressants and antipsychotics: SSRIs like citalopram and tricyclics like amitriptyline can disrupt heart rhythms. Antipsychotics like haloperidol and ziprasidone carry black box warnings from the FDA for this reason.
- Digoxin: Used for heart failure and atrial fibrillation, digoxin toxicity causes irregular rhythms - especially when blood levels go above 2 ng/mL. Kidney problems and low magnesium make this much more likely.
- Beta-blockers: While they slow the heart rate to help with atrial fibrillation, too much can cause dangerous bradycardia. Symptoms like dizziness, fatigue, or fainting may mean the dose is too high.
- Cancer drugs: Trastuzumab (Herceptin) and other targeted therapies can trigger atrial fibrillation through inflammation and oxidative stress, affecting 2-5% of patients.
What makes things worse is polypharmacy - taking multiple drugs at once. If you’re on two or more QT-prolonging medications, your risk jumps 300-500% compared to taking just one. That’s why it’s critical to review every medication you’re on, including over-the-counter and herbal products.
Warning Signs You Can’t Ignore
Most people don’t feel a dangerous arrhythmia coming until it’s already happening. But there are clear red flags that show up before things get critical:
- Palpitations: That fluttering, pounding, or skipping feeling in your chest. Reported by 70-80% of people who develop drug-induced arrhythmias.
- Dizziness or lightheadedness: Especially when standing up. This often means your heart isn’t pumping enough blood to your brain.
- Fatigue: Unexplained exhaustion that doesn’t improve with rest. This can be a subtle sign your heart is struggling.
- Chest discomfort: Not always a classic heart attack pain - sometimes it’s just pressure, tightness, or a strange ache.
- Fainting (syncope): The most serious warning. If you pass out unexpectedly, especially after starting a new medication, get checked immediately.
These symptoms don’t always mean you’re in immediate danger. But they’re your body’s way of saying something’s off. Don’t brush them off as stress or aging. Especially if they started after you began a new drug.
Who’s at Highest Risk?
Not everyone who takes these drugs will have problems. But certain factors make you much more vulnerable:
- Age 65 or older: About 60-70% of severe cases occur in older adults. Aging slows drug clearance and increases sensitivity to side effects.
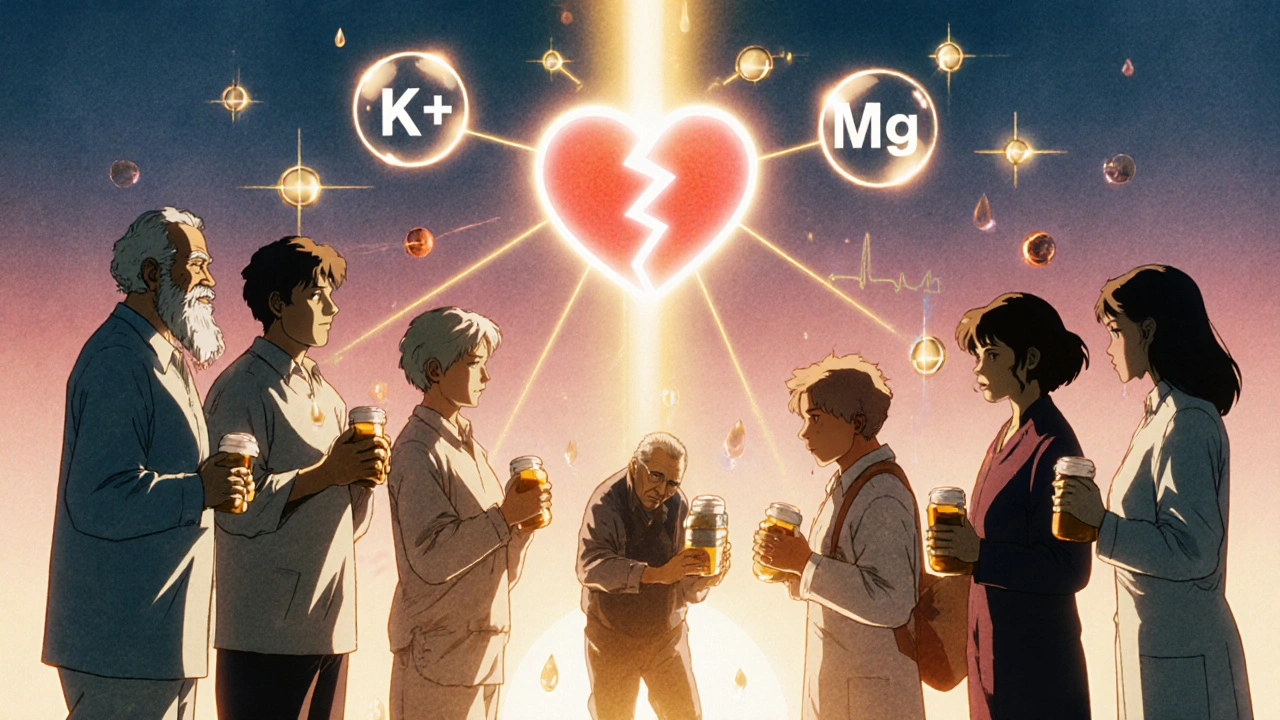
- Electrolyte imbalances: Low potassium (hypokalemia) affects 20% of hospitalized patients. Low magnesium (hypomagnesemia) affects 10-15%. Both make the heart more prone to dangerous rhythms.
- Chronic kidney disease: Impaired kidneys can’t clear drugs properly, leading to toxic buildup. Up to 40% of elderly patients on digoxin have some kidney impairment.
- Excessive alcohol: More than three drinks a day triples your risk. Alcohol directly damages heart tissue and depletes magnesium.
- Genetic factors: Around 15% of people of African ancestry carry the S1103Y variant. About 12% of East Asians carry R1193Q. These variants make heart cells far more sensitive to QT-prolonging drugs - even at normal doses.
If you’re on a high-risk medication and have any of these risk factors, your doctor should be monitoring you closely. If they’re not, ask why.
How Are These Arrhythmias Managed?
The good news: most drug-induced arrhythmias can be reversed if caught early. Here’s how it’s done in practice:
- Stop or adjust the medication: In 75-85% of cases, simply lowering the dose or switching to a safer alternative fixes the problem. For example, switching from citalopram to sertraline can eliminate QT prolongation without losing antidepressant benefits.
- Correct electrolytes: If potassium or magnesium is low, IV or oral supplements are given immediately. Target levels: potassium above 4.0 mEq/L and magnesium above 2.0 mg/dL.
- Monitor with ECG: Before starting high-risk drugs, get a baseline ECG. Repeat it within 72 hours. If the QT interval increases by more than 60 ms from baseline, the drug should be reconsidered.
- Use a pacemaker if needed: For patients on beta-blockers who develop dangerous bradycardia, a pacemaker allows them to keep the medication safely. About 10-15% of atrial fibrillation patients on rate-control drugs eventually need one.
- Catheter ablation: Needed in only 5-10% of persistent cases, this procedure destroys small areas of heart tissue causing the abnormal rhythm.
Surgery is rarely needed - less than 2% of cases. But ignoring the problem can be deadly. Drug-induced arrhythmias cause an estimated 100,000-150,000 hospitalizations in the U.S. each year, costing over $1.2 billion.
What You Can Do Right Now
You don’t need to wait for symptoms to get worse. Here’s what you can do today:
- Make a full medication list: Include prescriptions, OTC drugs, supplements, and herbal remedies. Bring it to every doctor visit.
- Ask: “Could this drug affect my heart rhythm?” Especially if you’re over 65, have kidney issues, or take multiple meds.
- Know your electrolytes: If you’re on diuretics or have had vomiting/diarrhea, ask for a blood test to check potassium and magnesium.
- Limit caffeine and alcohol: Caffeine triggers palpitations in 25-30% of people. Alcohol increases risk by 200-300%. Cutting back helps.
- Get an ECG if you have symptoms: A simple 10-second test can reveal QT prolongation or other abnormalities.
Don’t stop your meds on your own. But do speak up. The Texas Cardiac Arrhythmia Institute found that 65-75% of severe outcomes could be prevented with earlier recognition and action.
The Future: Personalized Medicine Is Coming
Right now, doctors often guess which patients are at risk. But that’s changing. Researchers are developing tools that predict your personal risk based on your genetics, age, kidney function, and current meds.
The American College of Cardiology is launching a clinical decision tool in 2024 that calculates your individual arrhythmia risk before prescribing. It will flag high-risk combinations and suggest safer alternatives. Meanwhile, genetic testing for variants like S1103Y and R1193Q is becoming more accessible. In the next five years, experts predict a 30-40% drop in severe cases thanks to these advances.
For now, awareness is your best defense. Know your meds. Know your body. And never ignore a weird heartbeat.
Can over-the-counter medications cause heart arrhythmias?
Yes. Many common OTC drugs can trigger arrhythmias. Antihistamines like diphenhydramine (Benadryl), decongestants like pseudoephedrine, and anti-nausea meds like dimenhydrinate (Dramamine) can prolong the QT interval. Even some herbal supplements - like licorice root or ephedra - carry risks. Always check with your pharmacist or doctor before taking new OTC products, especially if you’re on heart medication or have a history of rhythm problems.
Is it safe to take antibiotics if I have a heart condition?
It depends. Macrolides like azithromycin and fluoroquinolones like levofloxacin carry known risks for QT prolongation. If you have a history of arrhythmias, long QT syndrome, or are on other heart medications, your doctor may choose a safer alternative like amoxicillin or doxycycline. Never assume an antibiotic is harmless - always ask about cardiac risks before starting.
How do I know if my ECG shows QT prolongation?
Your doctor or cardiologist will measure the QT interval on your ECG. A normal QT interval is under 440 milliseconds for men and under 460 ms for women. If it’s over 500 ms, the risk of torsades de pointes becomes significant. Even a rise of more than 60 ms from your baseline ECG is a red flag. Ask for a copy of your ECG and the QT measurement - don’t wait for them to bring it up.
Can caffeine cause dangerous arrhythmias?
Caffeine alone rarely causes life-threatening arrhythmias. But it can trigger palpitations in 25-30% of people, especially if you’re sensitive or already on a QT-prolonging drug. For most, one or two cups of coffee a day is fine. But if you’re on an antidepressant or antibiotic known to affect heart rhythm, cutting back on caffeine can reduce your risk. Avoid energy drinks - they often contain high doses of caffeine plus other stimulants that compound the danger.
What should I do if I faint after starting a new medication?
Seek medical attention immediately. Fainting (syncope) after starting a new drug is a major red flag for a serious arrhythmia. Don’t wait to see if it happens again. Go to an emergency department or call your doctor right away. Bring your medication list. You may need an ECG, blood tests for electrolytes, and possibly a heart monitor. Early intervention can prevent a second, potentially fatal episode.

Comments (9)
Nick Lesieur November 19 2025
lol so now i gotta check every damn pill i take? even my benadryl? 😑
Angela Gutschwager November 20 2025
My grandma took Benadryl for 20 years. She never fainted. Maybe it’s not the drug-it’s the overmedicated culture.
Dion Hetemi November 21 2025
Let’s be real-this is just Big Pharma’s way of making you paranoid so you’ll buy more ‘safe’ drugs. They profit when you’re scared. The real danger? Not knowing your own body. You’re not a machine. Your heart isn’t a circuit board. Stop treating it like one.
Andy Feltus November 23 2025
It’s funny how we treat medicine like magic spells-take it, and everything’s fixed. But the body’s not a vending machine. You put in a pill, you get a result. It’s an ecosystem. And when you throw in a dozen chemicals, you’re not just treating a symptom-you’re playing Jenga with your autonomic nervous system. And someone’s always gonna pull the wrong block.
river weiss November 23 2025
Baseline ECG before starting any QT-prolonging agent is non-negotiable. Especially in patients over 65, with renal impairment, or on polypharmacy. I’ve seen too many avoidable hospitalizations because this wasn’t done. Always document QT interval. Always. And if your doctor doesn’t mention it-ask. It’s your right.
Kara Binning November 24 2025
I’m so tired of this medical gaslighting. I passed out after my new antidepressant. Doctor said, ‘It’s probably anxiety.’ I had a 520ms QT. They didn’t even check. Now I have a pacemaker. This isn’t ‘awareness’-this is negligence. And now they want me to ‘speak up’? I should’ve been screaming before I collapsed.
Brian Rono November 26 2025
Oh, so now diphenhydramine is the new nicotine? Next they’ll ban caffeine, chocolate, and sunlight because ‘it might trigger arrhythmias in susceptible individuals.’ This isn’t medicine-it’s fearmongering wrapped in a white coat. If you’re healthy, stop treating every pill like a landmine.
Zac Gray November 27 2025
Look-I get it. The system’s broken. Doctors are rushed. Patients are handed scripts like candy. But here’s the thing: you don’t need to be a cardiologist to be your own advocate. Keep a log: what you took, when, and how you felt. Did your heart skip after the antibiotic? Did you feel dizzy after the new painkiller? Write it down. Bring it in. Be the person who says, ‘I noticed something.’ That’s how you save your life. And if your doctor rolls their eyes? Find a new one. Your heart doesn’t care about their schedule.
James Ó Nuanáin November 27 2025
As a British physician with 27 years in cardiology, I must emphasize that the rise in drug-induced arrhythmias is directly correlated with the erosion of clinical judgment in favor of algorithmic prescribing. The FDA black box warnings exist for a reason. The fact that patients are now expected to self-diagnose QT prolongation via ECGs they don’t understand is not innovation-it is institutional failure. In the NHS, we still prioritize clinical correlation over digital noise. If your potassium is below 4.0, no medication should be initiated without correction. Period. This isn’t opinion-it is evidence-based protocol. And yes, I have seen patients die because someone thought ‘it was just anxiety.’