When you’re managing type 2 diabetes, finding a medication that lowers blood sugar and protects your heart is a win. But for some people taking canagliflozin (brand name INVOKANA®), that win came with a hidden cost: an increased risk of losing a toe, foot, or even part of a leg. This isn’t fear-mongering. It’s data. And it’s real.
What Happened with Canagliflozin?
Canagliflozin was approved in 2013 as part of a new class of diabetes drugs called SGLT2 inhibitors. These drugs work by making your kidneys flush out extra sugar through urine - a clever trick that lowers blood glucose without causing weight gain or low blood sugar. Early studies showed it also reduced heart failure and kidney damage in high-risk patients. That’s why it quickly became popular. Then, in 2017, the CANVAS Program - a major clinical trial involving over 10,000 people - dropped a bombshell. People taking canagliflozin were more than twice as likely to have a lower-limb amputation compared to those on placebo. The numbers were stark: 5.5 amputations per 1,000 patient-years at the higher dose (300 mg), versus 2.8 in the placebo group. Most were minor - toes or parts of the foot - but 20% were major, above the ankle. The FDA responded immediately. They added a boxed warning - the strongest possible alert - to the drug label. Doctors were told to avoid prescribing it to patients with poor circulation, foot ulcers, or nerve damage. Many stopped using it altogether.But Then… The Warning Was Removed
By early 2020, the FDA quietly removed the boxed warning. Not because the risk disappeared. But because they re-evaluated everything - including the CREDENCE trial, which showed canagliflozin dramatically slowed kidney disease progression in people with diabetic nephropathy. The benefits, especially for high-risk kidney patients, were too big to ignore. Today, the risk is still there. It’s just no longer labeled as a “boxed warning.” Instead, it’s clearly stated in the Warnings and Precautions section of the prescribing information. The FDA still says: “Monitor for new pain, tenderness, sores, ulcers, or infections in the legs or feet.” And they mean it.Is This Risk Unique to Canagliflozin?
This is the most important question. And the answer is yes - at least for now. Other SGLT2 inhibitors like empagliflozin (Jardiance) and dapagliflozin (Farxiga) have been studied just as hard. In the EMPA-REG OUTCOME trial, empagliflozin showed no increased amputation risk. In fact, dapagliflozin’s DECLARE-TIMI 58 trial showed a slight trend toward fewer amputations. A 2023 meta-analysis of over 74,000 patients confirmed: only canagliflozin had a statistically significant link to amputation. Why? We don’t fully know. But clues point to how canagliflozin affects the body. It lowers blood pressure more than other drugs in its class - by about 3.7 mmHg systolic. It also causes greater weight loss - nearly 3 kg on average. In people with already compromised circulation, that drop in pressure and volume might reduce blood flow to the feet just enough to turn a small sore into a life-altering problem.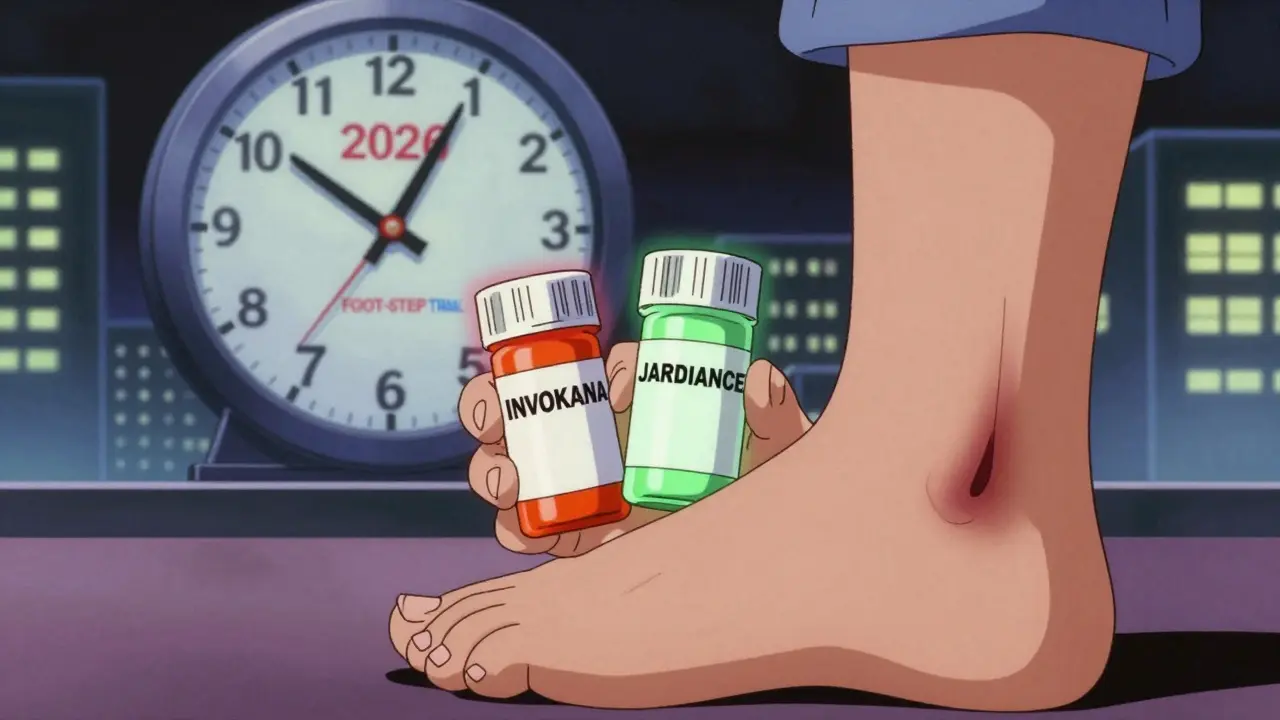
Who’s Really at Risk?
Not everyone on canagliflozin will have an amputation. The absolute risk is low. One study estimated that for every 556 people treated for a year, only one extra amputation occurs. That’s rare. But rare doesn’t mean harmless - especially if you’re in the high-risk group. The real danger lies in pre-existing conditions:- Peripheral artery disease (PAD) - present in 20-30% of people with type 2 diabetes
- Diabetic neuropathy - affects up to half of all patients
- History of foot ulcers - 40% of those who’ve had one will get another within a year
- Smoking - doubles the risk of poor circulation
- Prior amputation - the single biggest predictor of future amputation
What Should You Do If You’re on Canagliflozin?
If you’re already taking it, don’t panic. But do take action. 1. Get a foot exam - now. Your doctor should check for pulses, sensation, skin changes, and any sores. If you haven’t had one in the last 6 months, schedule one. The American Diabetes Association now recommends an ankle-brachial index (ABI) test before starting canagliflozin if you have any cardiovascular risk factors. An ABI below 0.9 means poor leg circulation - and it’s a red flag. 2. Check your feet daily. Use a mirror. Look between toes. Feel for warmth, swelling, or new pain. Even a small blister can turn into an ulcer if you have nerve damage and don’t feel it. The NICE guidelines say: “Report any new foot problem immediately - don’t wait.” 3. Talk to your doctor about alternatives. If you have risk factors, switching to empagliflozin or dapagliflozin may be safer. Both have proven heart and kidney benefits without the amputation signal. Jardiance and Farxiga are now the go-to SGLT2 inhibitors for most clinicians. 4. Know the signs. Redness, swelling, warmth, drainage, odor, or non-healing sores? Don’t wait for your next appointment. Call your podiatrist or endocrinologist. Time is tissue.Real Stories - Not Just Numbers
On PatientsLikeMe, 6.9% of canagliflozin users reported foot problems. A Reddit user named u/DiabetesWarrior2020 shared: “After 18 months on Invokana, my podiatrist found a non-healing ulcer. I lost my toe. My endocrinologist switched me to Jardiance the next day.” Another user, u/SugarFreeLife, wrote: “Three years on Invokana. No foot issues. My A1c dropped from 8.5% to 6.2%.” Both are true. That’s the problem - and the solution. It’s not about the drug being “bad.” It’s about matching the right drug to the right person.
What’s Changing Now?
The landscape is shifting. In January 2024, the FDA required all SGLT2 inhibitors to include standardized foot care counseling in their medication guides. That means every prescription now comes with clear instructions on foot checks and warning signs. Janssen, the maker of INVOKANA, is testing a new extended-release version (INVOKANA XR) that may reduce peak drug levels - and possibly lower the amputation risk. Early data is promising. The FOOT-STEP trial, running until 2026, is testing whether structured foot care programs - weekly check-ins, custom footwear, rapid ulcer treatment - can prevent amputations in high-risk patients on canagliflozin. Results could change everything.The Bottom Line
Canagliflozin is not banned. It’s not evil. It’s a powerful tool - but only for the right patient. For someone with heart failure, kidney disease, and no foot problems? It can be life-saving. For someone with numb feet, smoking, and poor circulation? It’s a gamble you shouldn’t take. The key isn’t avoiding the drug entirely. It’s knowing who it’s safe for - and who it’s not. If you’re on canagliflozin, ask your doctor: “Do I have any risk factors for foot problems?” If you’re considering it, ask: “Is this the safest SGLT2 inhibitor for me?” The data is clear. The tools are there. And the choice? That’s yours - with the right information.Is canagliflozin still prescribed today?
Yes, but more cautiously. In 2023, canagliflozin made up 22% of SGLT2 inhibitor prescriptions in the U.S., down from 35% in 2017. Doctors now avoid it in patients with foot ulcers, poor circulation, or neuropathy. It’s still used in patients with heart or kidney disease who don’t have those risk factors.
How common are amputations with canagliflozin?
Very rare overall. About 5.5 out of every 1,000 people taking the 300 mg dose had an amputation per year - compared to 2.8 per 1,000 on placebo. That’s roughly 1.8 extra amputations per 1,000 patient-years. But for people with existing foot problems, the risk is much higher.
Are all SGLT2 inhibitors equally risky?
No. Only canagliflozin has shown a consistent, statistically significant increase in amputation risk. Empagliflozin (Jardiance) and dapagliflozin (Farxiga) have not shown this signal in major trials. Many doctors now prefer these alternatives for patients with any foot or circulation concerns.
What should I do if I notice a sore on my foot while taking canagliflozin?
Call your doctor or podiatrist immediately. Don’t wait. Even a small blister can become a serious infection if you have nerve damage. Early treatment - cleaning, offloading pressure, antibiotics if needed - can prevent amputation. The FDA and NICE both stress: report foot changes right away.
Can I switch from canagliflozin to another diabetes drug safely?
Yes, and many people do - especially if they have foot or circulation issues. Empagliflozin and dapagliflozin are common switches. Both offer similar blood sugar control and heart/kidney benefits without the amputation signal. Your doctor will monitor your blood sugar closely during the transition.
Does the FDA still consider canagliflozin safe?
The FDA removed the boxed warning in 2020 after reviewing more data, but it still lists amputation risk in the Warnings and Precautions section. They say the benefits outweigh the risks for certain patients - especially those with kidney disease - but only if foot health is monitored. They now require all SGLT2 inhibitors to include foot care education in their packaging.


Comments (15)
Bennett Ryynanen December 30 2025
Bro, I lost my toe on this drug. No joke. Wasn't even smoking, no ulcers, just numb feet from diabetes. Doctor swore it was fine. Turns out, the FDA warning was buried in the tiny print. Now I walk with a cane and a chip on my shoulder. Don't let them gaslight you into thinking it's 'rare' - if it happens to you, it's 100%.
Hanna Spittel December 31 2025
Big Pharma’s latest scam. They knew. They ALWAYS knew. Why do you think the boxed warning vanished? Because they rebranded the risk as ‘patient responsibility.’ Wake up. They profit from amputations. Think about it.
Deepika D January 2 2026
Let me tell you something - I’m a diabetes educator in Bangalore, and I’ve seen this play out too many times. Canagliflozin? It’s like giving someone a Ferrari with bald tires and telling them to ‘just drive carefully.’ The drug works wonders for kidney and heart - no doubt. But if your feet are already whispering ‘help,’ this isn’t the time to ignore the signs. I’ve had patients switch to Jardiance and literally feel like they got their life back - no more midnight panic checks for blisters. The key isn’t fear. It’s awareness. Get an ABI test. Check your feet daily. If your doctor doesn’t bring it up, ask. And if they roll their eyes? Find a new one. Your toes matter more than your HbA1c number.
Brady K. January 3 2026
Oh wow. So the FDA removed the boxed warning because the benefit-risk ratio improved? Wow. Groundbreaking. Next you’ll tell me that cigarettes were ‘re-evaluated’ and now only come with a ‘gentle reminder’ to not inhale. This isn’t science - it’s corporate arithmetic. They weighed a kidney save against a toe loss and said ‘eh, statistically, the toe doesn’t count.’ And now we’re supposed to pat them on the back for being ‘transparent’ in the Warnings section? Please. That’s like putting a ‘Caution: Hot Coffee’ label on a flamethrower.
Chandreson Chandreas January 4 2026
Life’s weird, right? 😅 One guy loses a toe, another drops 20 lbs and feels like a new person. Same drug. Different bodies. Maybe the real question isn’t ‘is it dangerous?’ but ‘who is it dangerous FOR?’ Like, should we ban all cars because someone got hit by a drunk driver? Nah. We just make sure people wear seatbelts and check their brakes. Canagliflozin’s the car. Your feet? The brakes. Check ‘em. Don’t ignore ‘em. 🚗👣
Kayla Kliphardt January 6 2026
Does anyone know if the new extended-release version (INVOKANA XR) has been tested on people with PAD or neuropathy? I’m trying to decide whether to switch, but I’m not sure if the new formulation changes the risk profile or just the dosing schedule.
Paul Huppert January 7 2026
My cousin’s on it. No issues. But she’s 58, active, no neuropathy, no smoking, good circulation. She gets her feet checked every 3 months. That’s the difference. It’s not the drug. It’s the context.
anggit marga January 8 2026
Why are Americans so scared of their feet? In Nigeria we just walk barefoot in the market and if something hurts we rub it with pepper and keep going. This is why your health system is broken. You overthink everything. Canagliflozin is fine. Stop being weak.
Urvi Patel January 8 2026
Look if you're not a medical doctor with a PhD in nephrology you have no business even discussing this. The meta-analysis is clear. The FDA re-evaluated. You're just spreading fear based on anecdotal Reddit posts. If you're worried, go to a specialist. Don't clutter the feed with your ignorance
Joy Nickles January 10 2026
Okay so I’m on this drug and I’ve had 3 foot sores in 14 months and my doctor keeps saying ‘it’s just dry skin’ and I’m like… is this normal?? I mean like I’m not diabetic for nothing I know what a sore looks like but they’re like ‘it’s probably just the medication’ and I’m like… IS IT?? HELP??
Emma Hooper January 10 2026
Y’all are acting like this is the first time a drug had a dark side. Remember fen-phen? Vioxx? Thalidomide? Drugs don’t come with a ‘perfect for everyone’ sticker. This one’s got a ‘use with caution’ tag - and if you’re the type who forgets to check your feet? Maybe don’t be the guinea pig. But if you’re sharp, disciplined, and got a good podiatrist? Go for it. Your kidneys will thank you. Your toes? Well… they’ll thank you too if you’re paying attention.
John Chapman January 10 2026
Just switched from Invokana to Jardiance last month. My A1c stayed the same. My foot numbness? Gone. My anxiety? Down 90%. I didn’t lose a toe. I didn’t even get a blister. Sometimes the best medicine is just… switching to something that doesn’t make you check your feet like a paranoid detective every night. 🙌
Frank SSS January 12 2026
Wow. So the real villain here isn’t the drug - it’s the patients who don’t check their feet. That’s the narrative? You’re telling me the solution to a drug-induced amputation risk is… more self-monitoring? That’s like saying the solution to lead paint is ‘just wash your hands more.’ The system failed. The drug failed. And now we’re blaming the victim for not being perfect? No thanks.
Robb Rice January 13 2026
As a physician who prescribes SGLT2 inhibitors, I can confirm: canagliflozin is still used - but only after documented ABI > 0.9, no active ulcers, and patient education signed off. The risk is real, but manageable. The key is not avoidance - it’s stratification. We’re not playing Russian roulette. We’re doing precision medicine. If you’re not being screened properly, that’s on your provider - not the drug.
Bennett Ryynanen January 13 2026
^This. My doctor didn’t screen me. That’s on him. Not the drug. But now I know. And I’m telling everyone. If your doc doesn’t mention ABI or pedal pulses before prescribing this - walk out. And take this post with you.